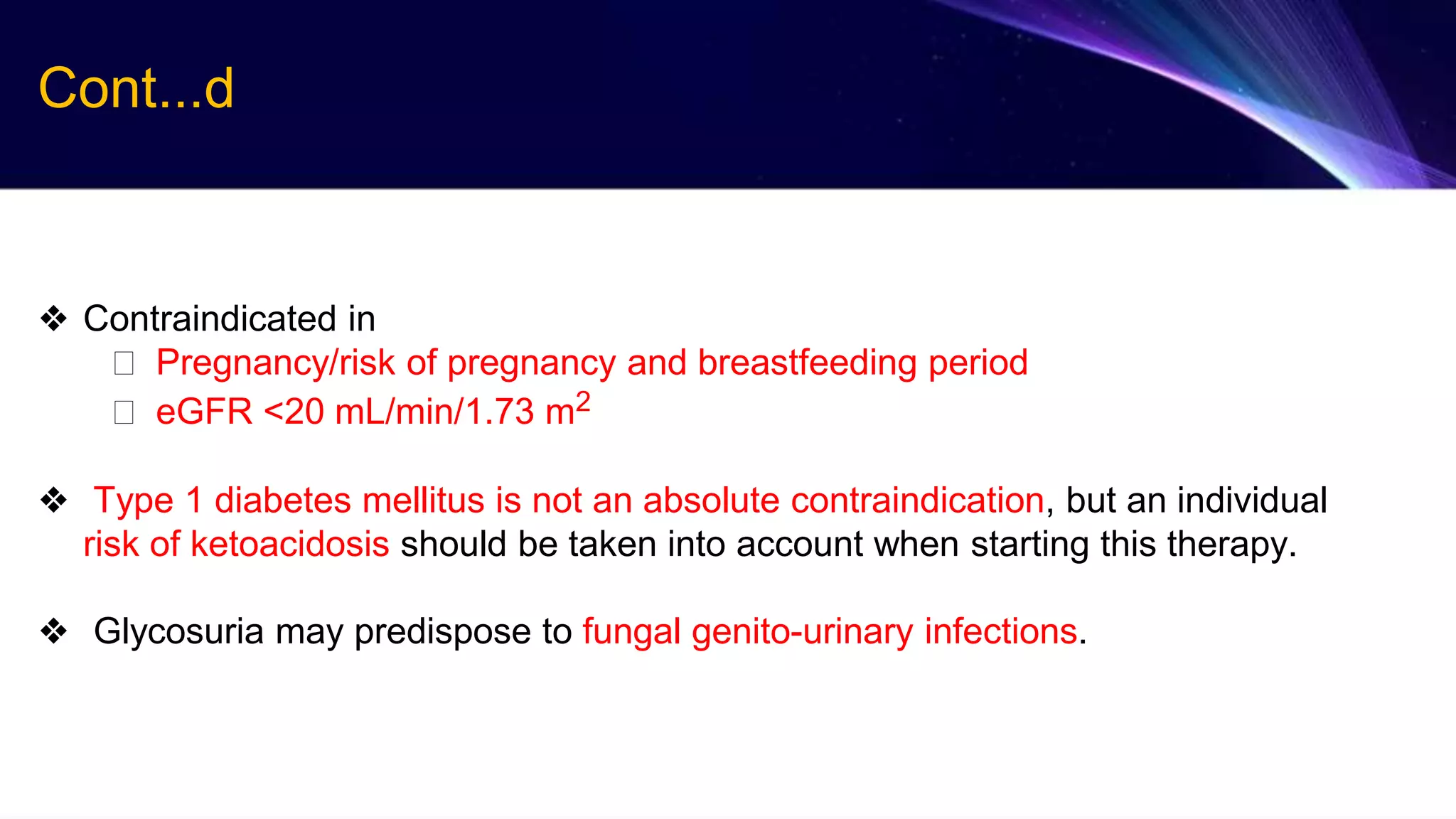
The 2021 ESC Guidelines for Heart Failure include several changes: a new term for HFmrEF, simplified treatment algorithms for HFrEF and according to phenotypes, modified classification for acute HF, and updated treatments for comorbidities. Key recommendations include treating HFrEF with ACE-I/ARNI, beta-blockers, MRAs, and SGLT2 inhibitors. For HFmrEF, ACE-I/ARNI, beta-blockers, and MRAs may be considered. Treatment of acute HF focuses on diuretics, inotropes, and short-term mechanical circulatory support.