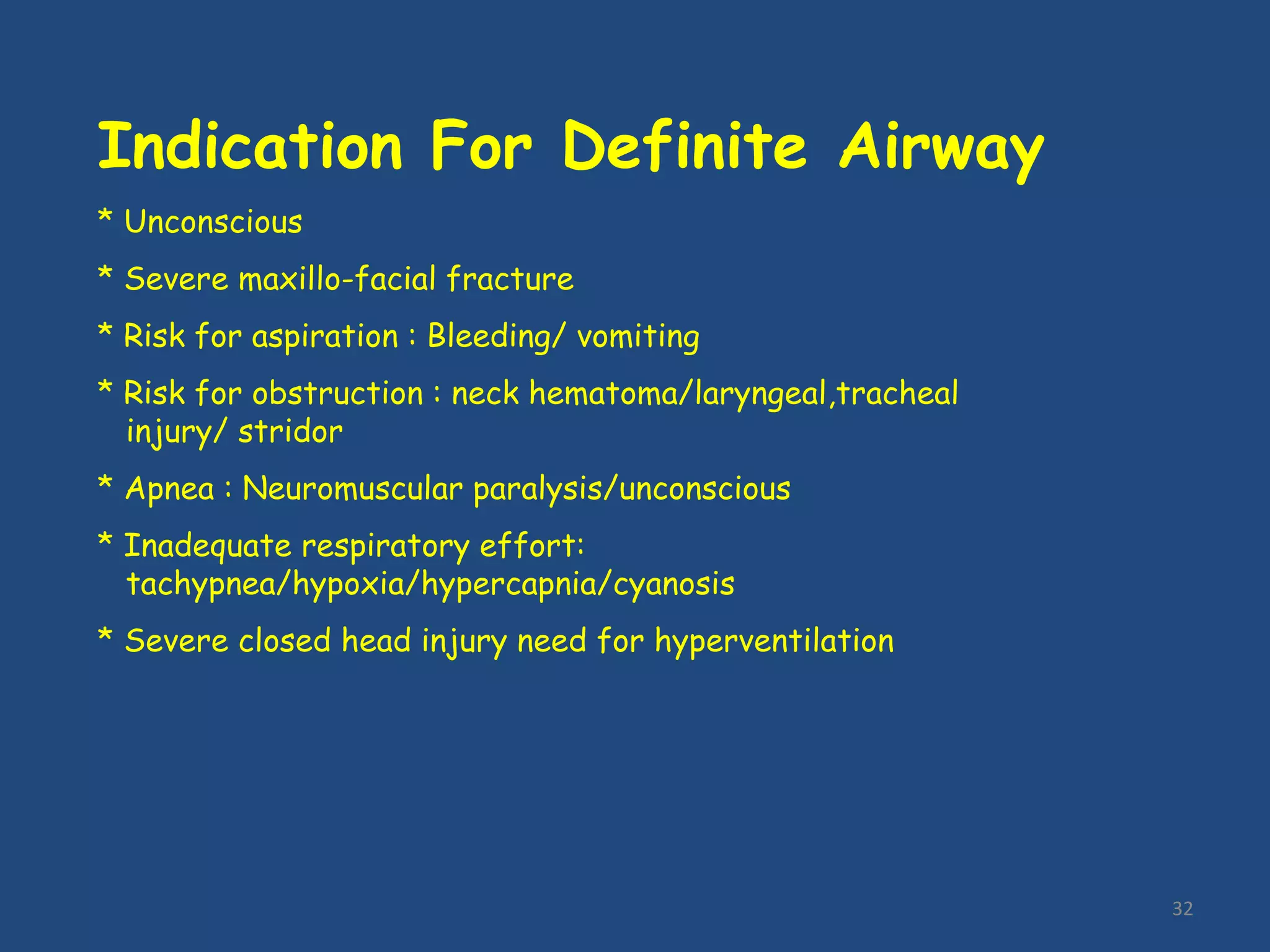
The document outlines the Advanced Trauma Life Support (ATLS) protocol for treating trauma patients. It describes the 9 steps of ATLS as: 1) Preparation, 2) Triage, 3) Primary Survey (ABCDE), 4) Resuscitation, 5) Adjuncts to primary survey & resuscitation, 6) Secondary Survey, 7) Adjuncts to secondary survey, 8) Continued post-resuscitation monitoring & re-evaluation, and 9) Definitive care. The primary and secondary surveys involve a head-to-toe examination to identify life-threatening injuries and provide initial stabilization of airway, breathing, circulation, disability, and exposure.