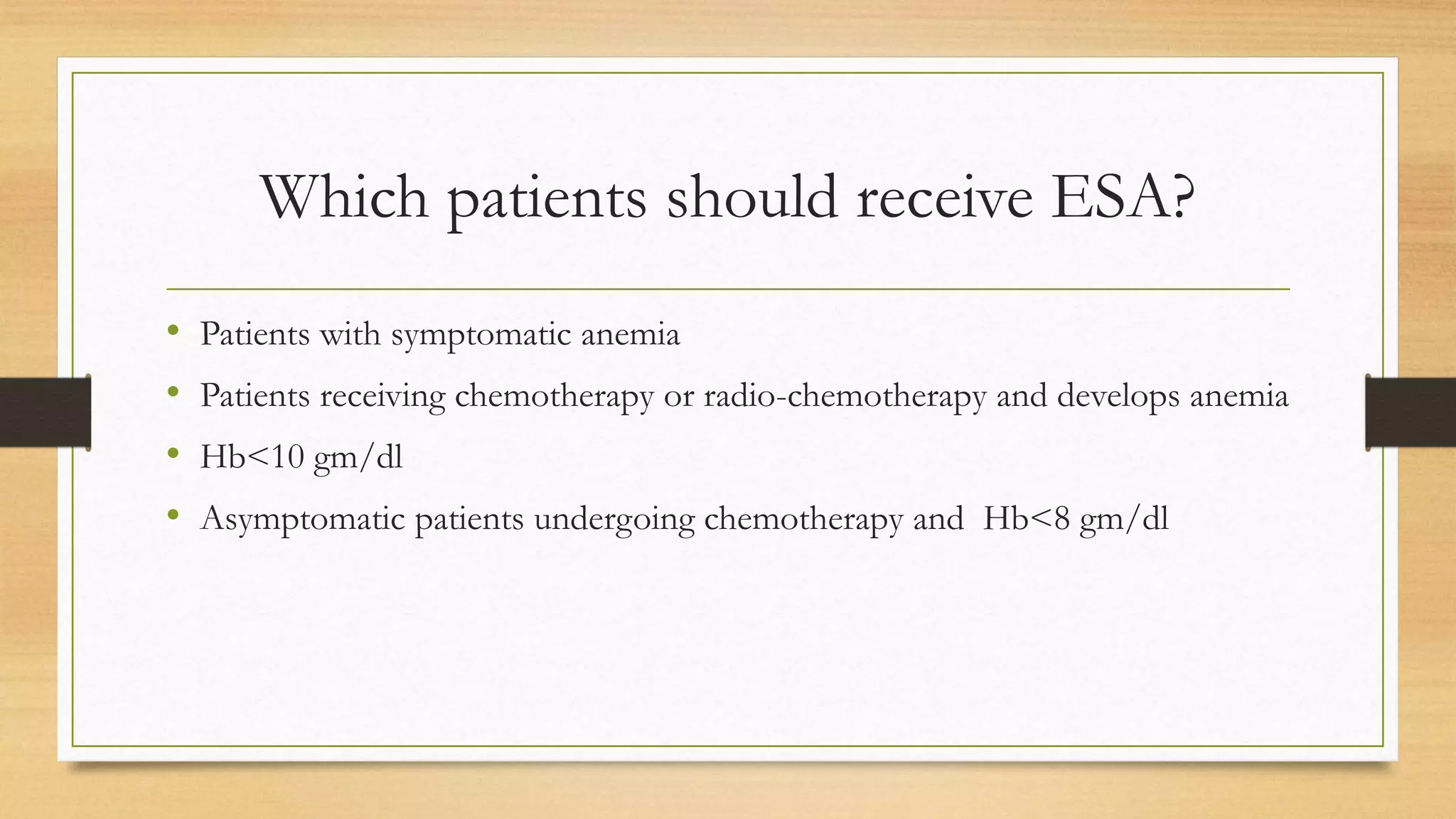
The document discusses anemia of chronic disease (ACD) and its relationship with various conditions such as chronic kidney disease and malignancies. It outlines causes, clinical features, evaluation methods, and treatment options including the use of erythropoietin-stimulating agents and iron supplementation. Anemia affects patient outcomes, particularly in those undergoing chemotherapy, necessitating careful management and monitoring.