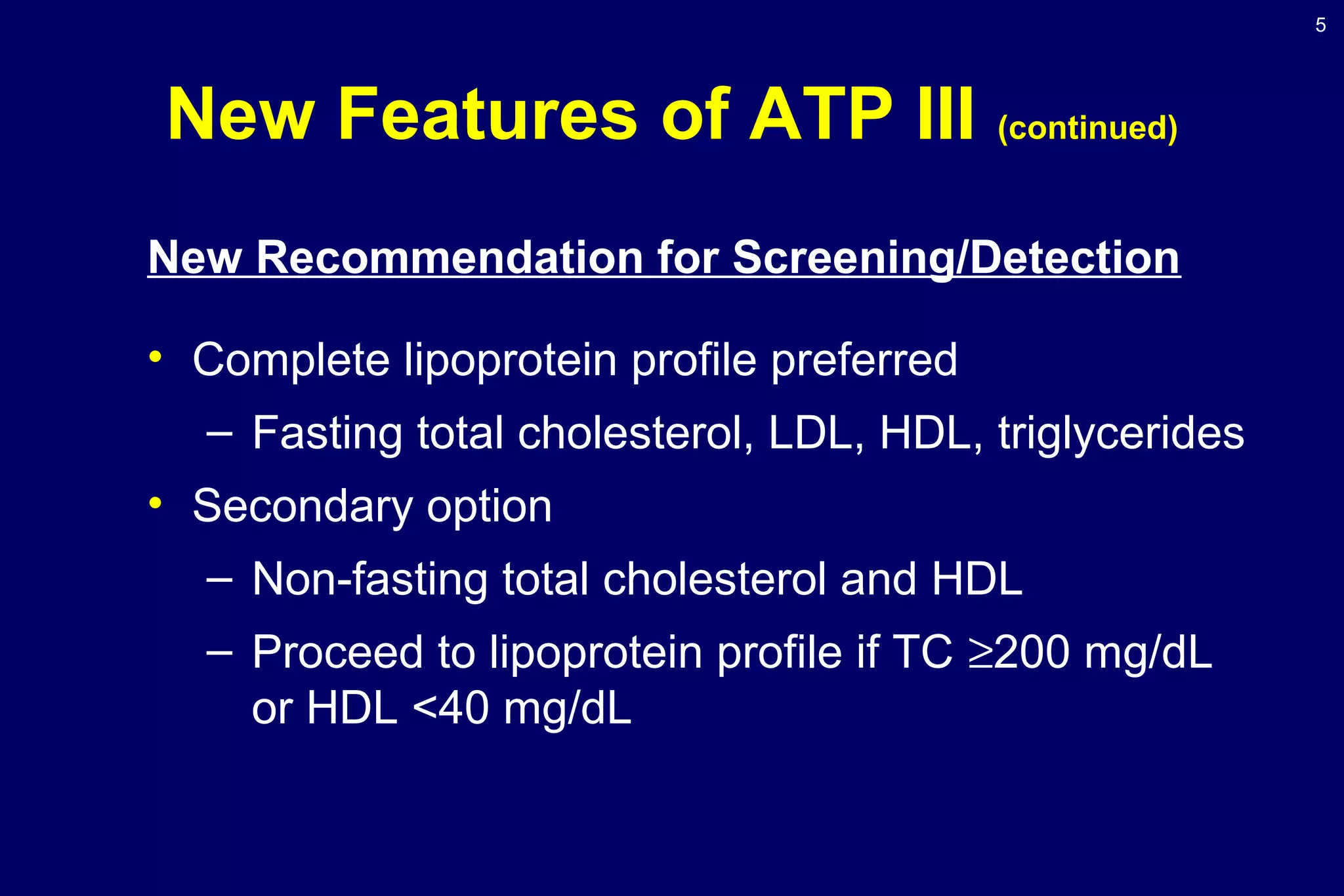
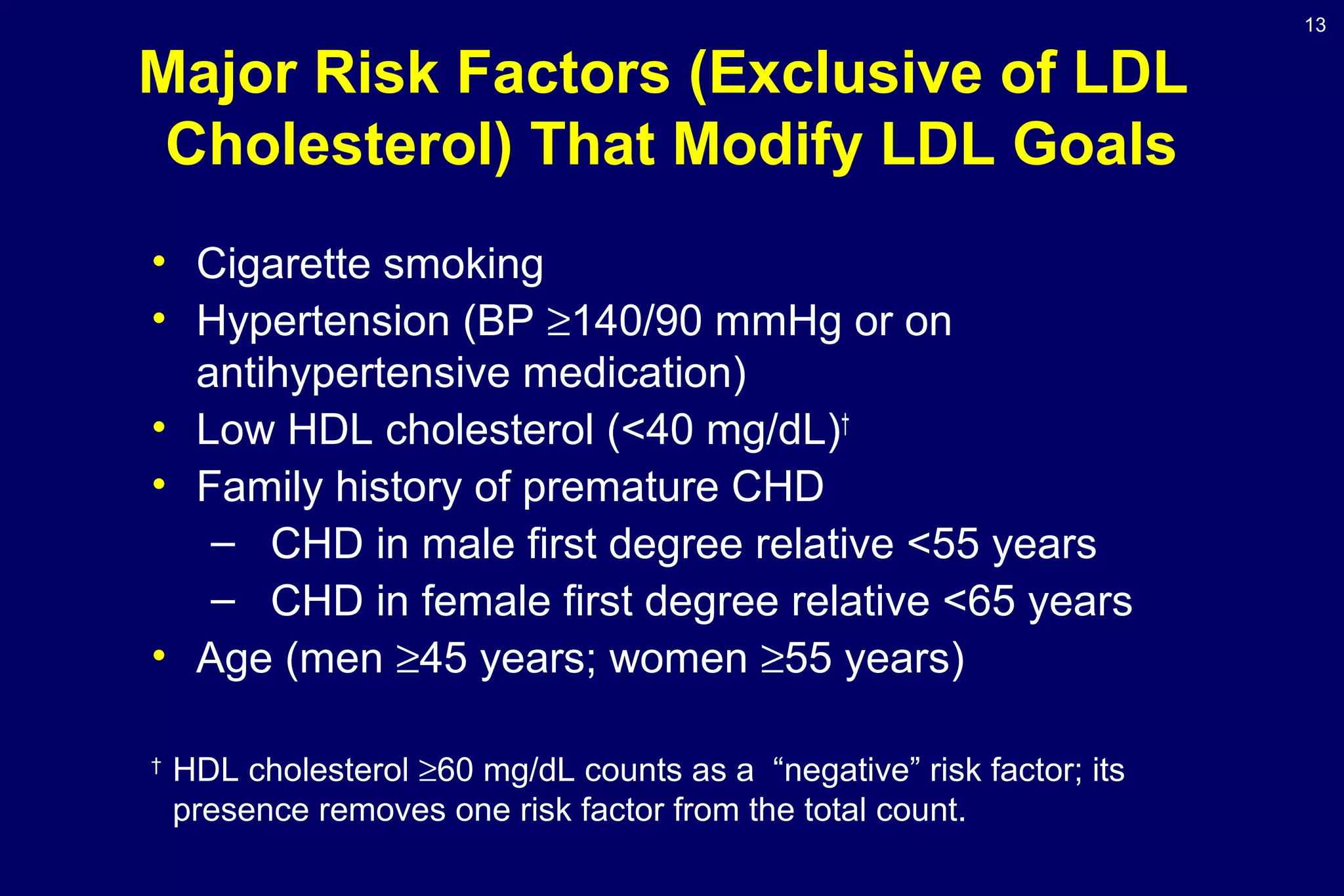
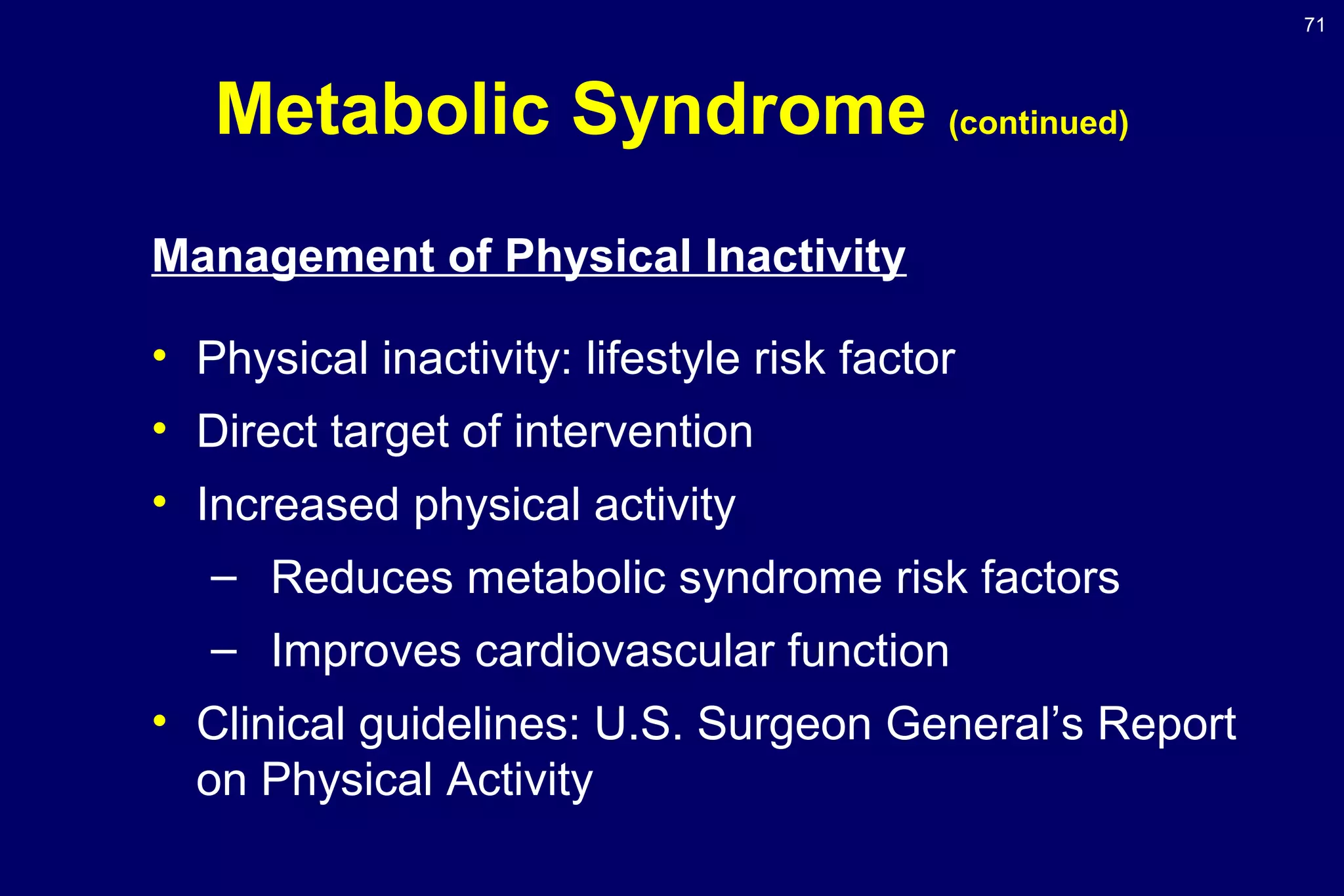
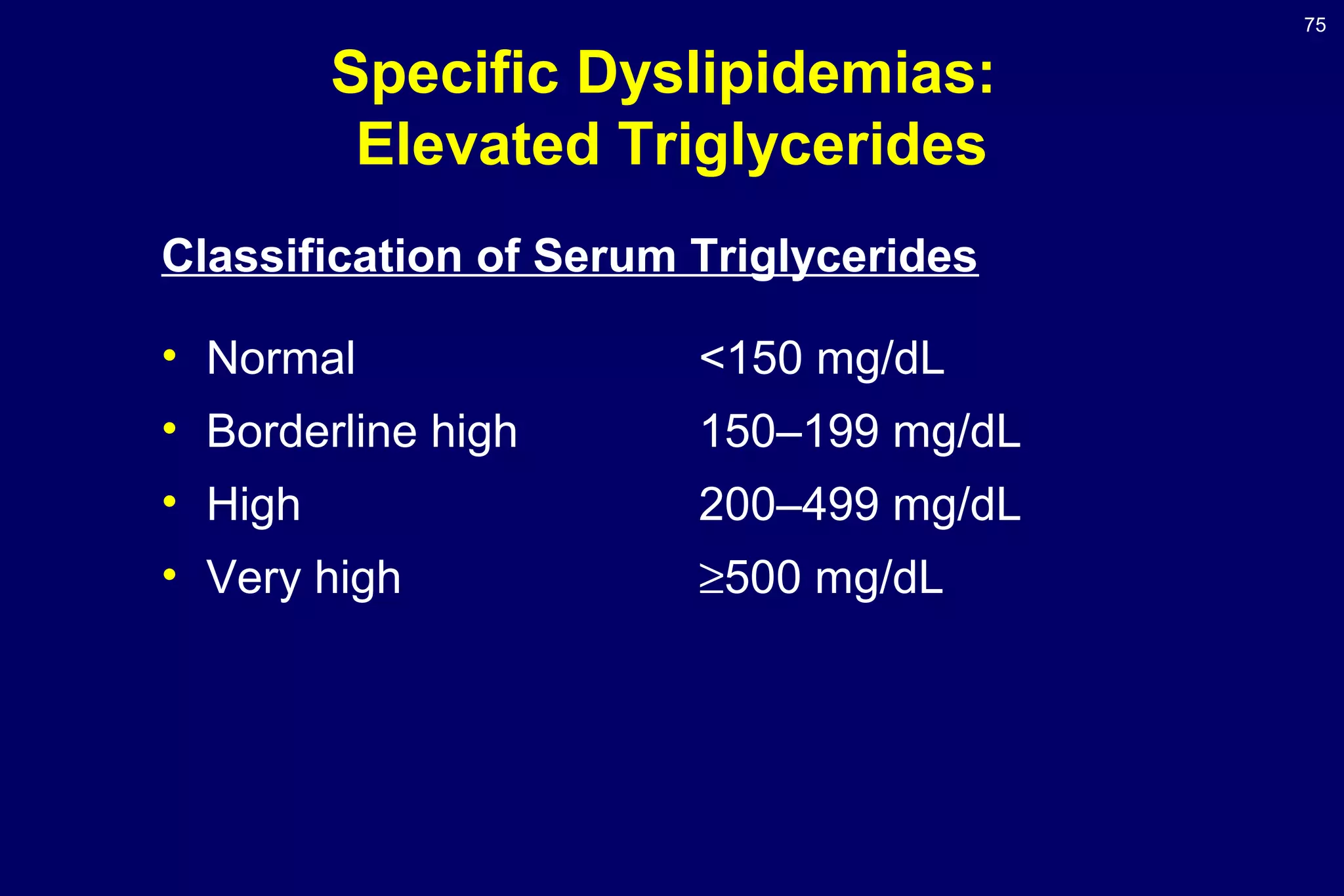
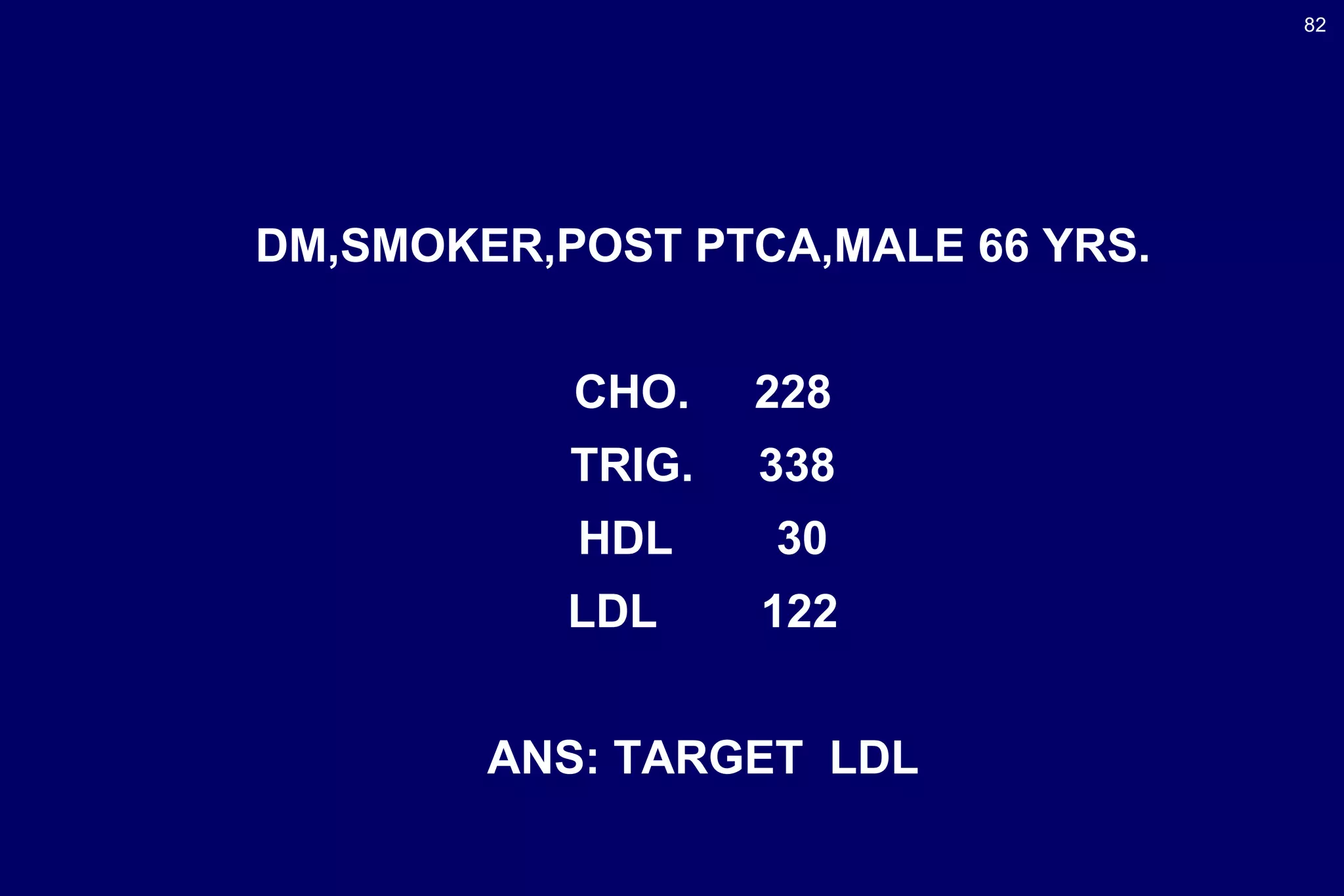
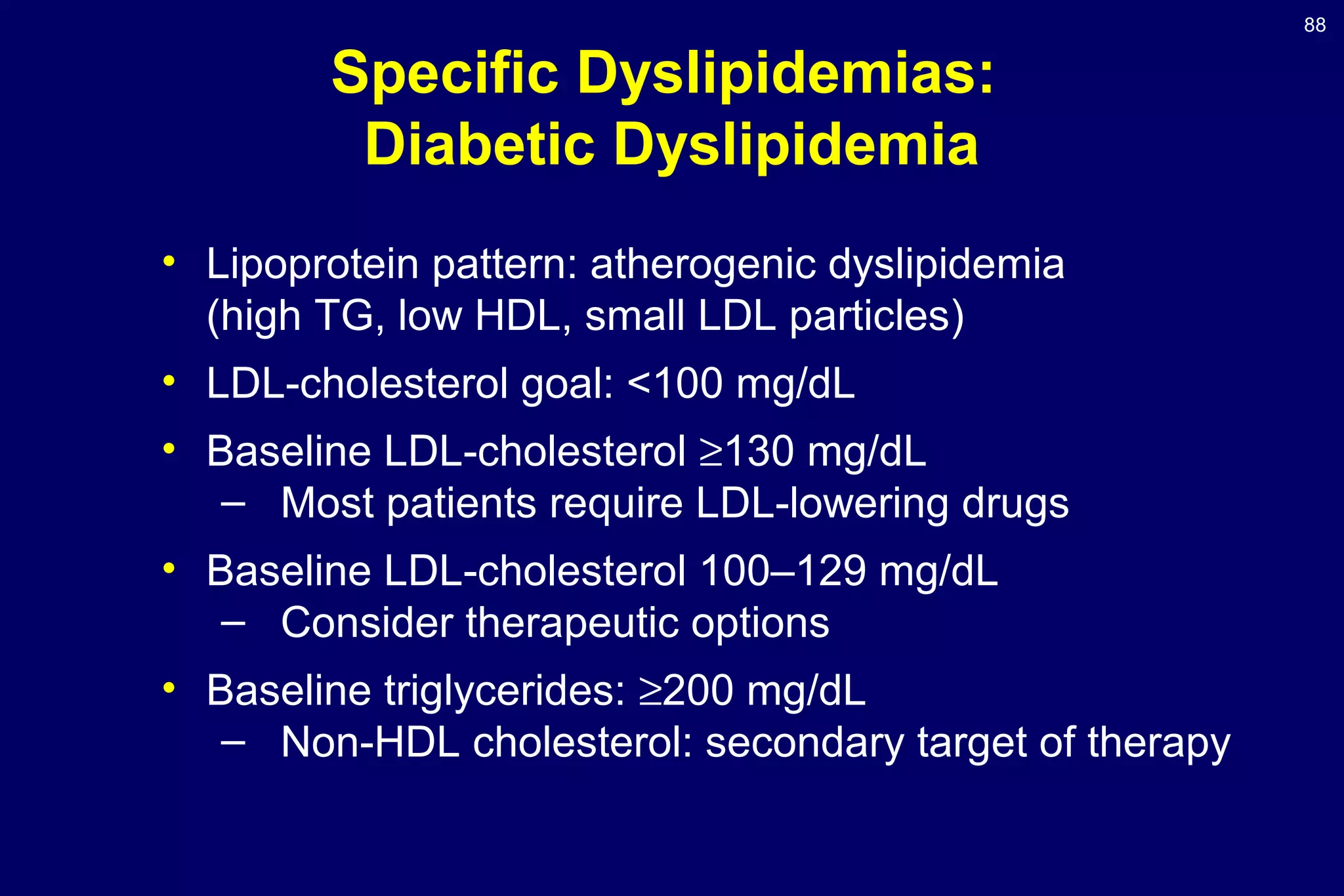
This document summarizes the key guidelines from the Adult Treatment Panel III (ATP III) on cholesterol treatment and prevention. The guidelines focus on multiple risk factors like diabetes, which is considered a cardiovascular disease risk equivalent. It modifies lipid classification cut-offs and recommends a complete lipoprotein profile for screening. It provides LDL cholesterol goals and criteria for lifestyle changes or drug therapy based on a patient's risk category of having cardiovascular disease, multiple risk factors, or 0-1 risk factor. The metabolic syndrome is highlighted as a secondary target of therapy beyond LDL lowering. Case examples are given to demonstrate how the guidelines would be applied.