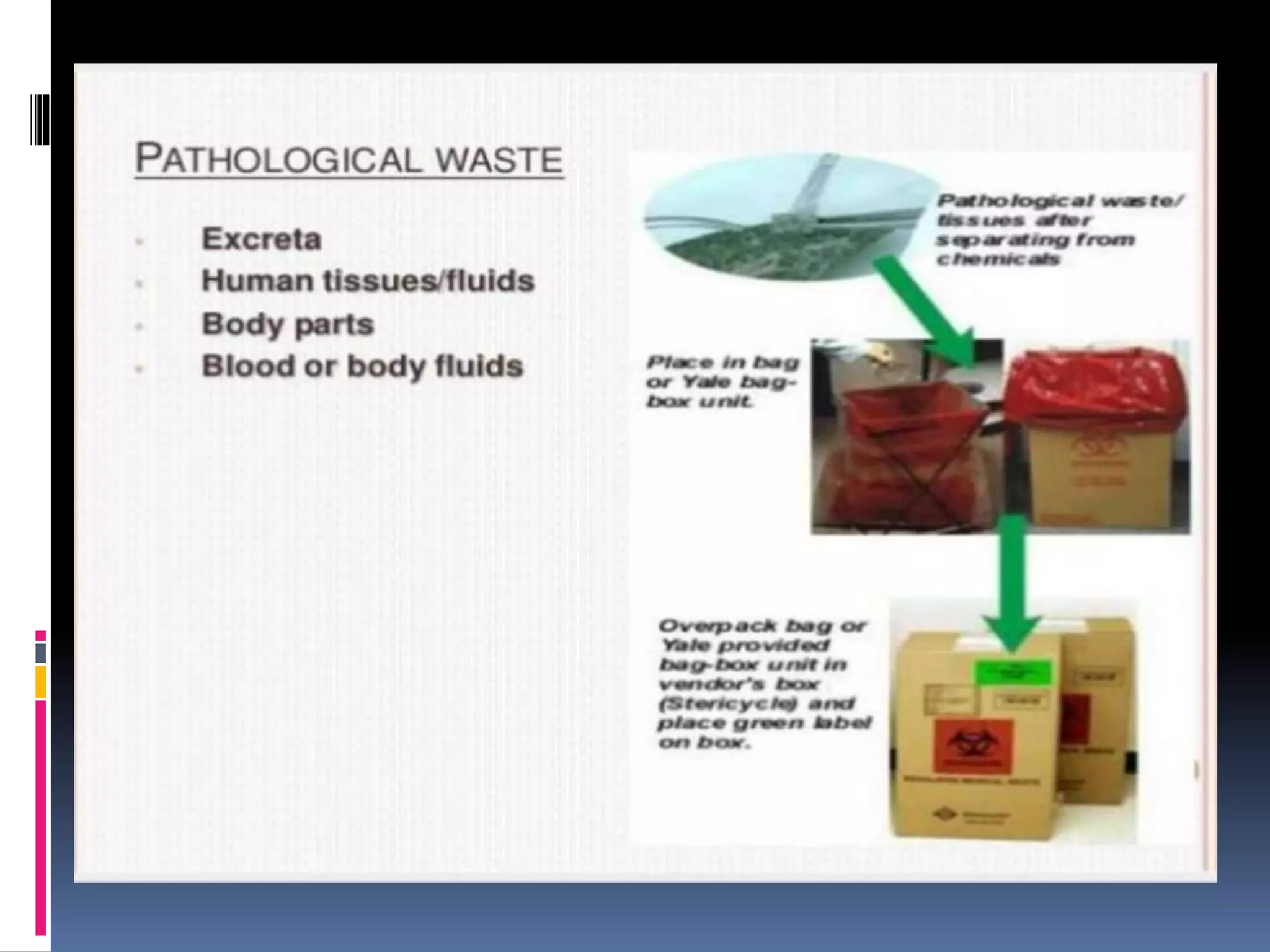
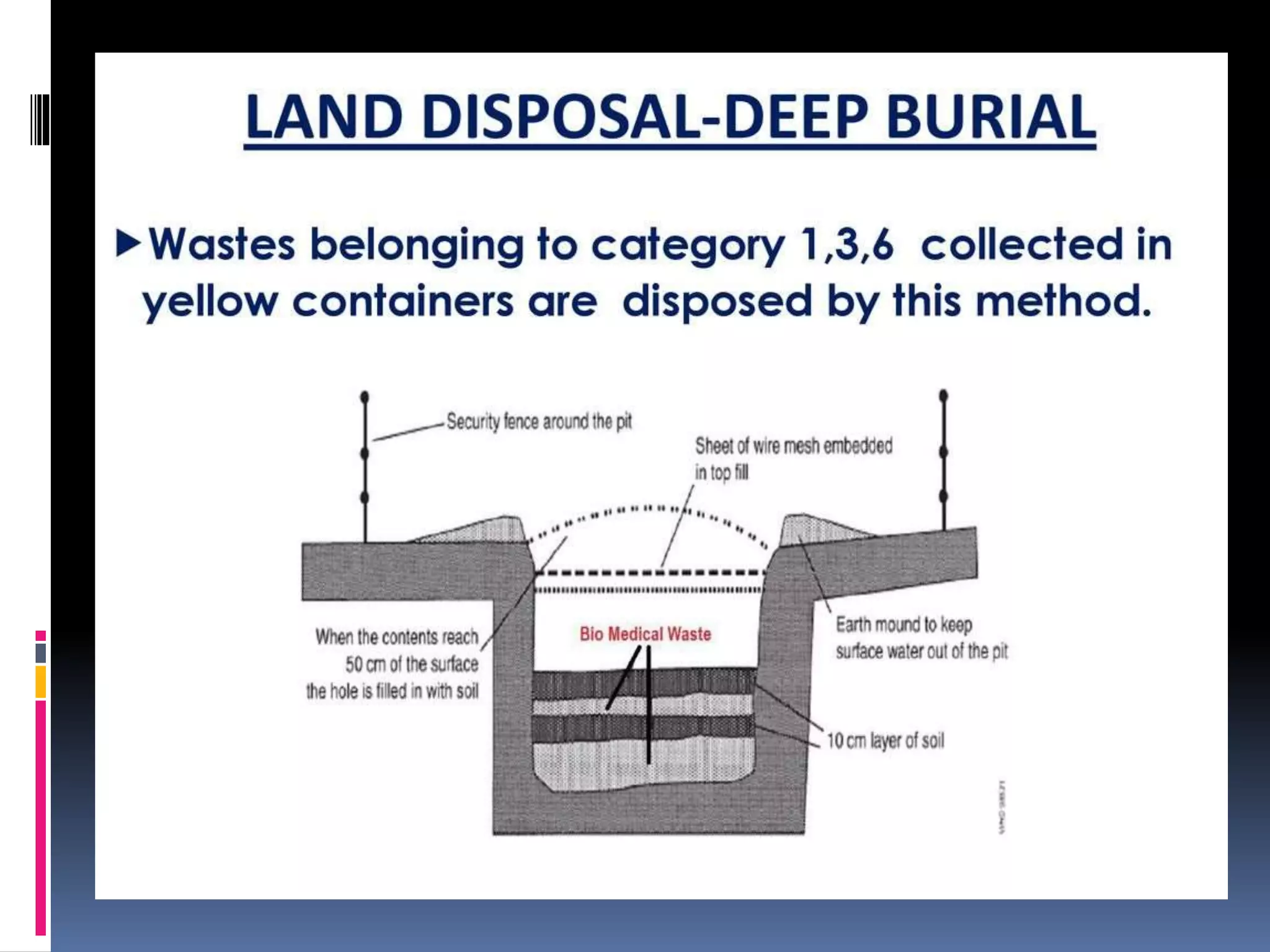
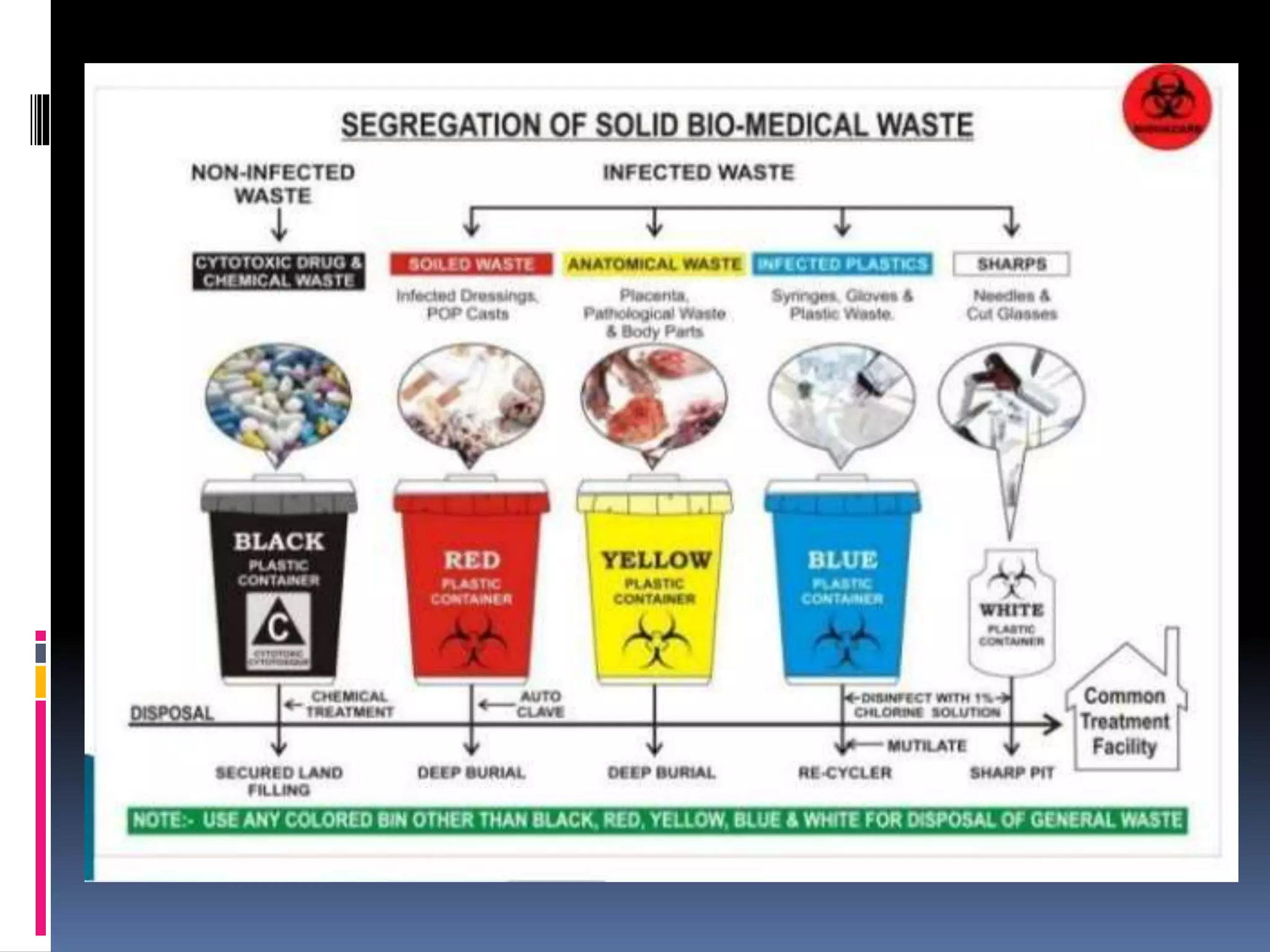
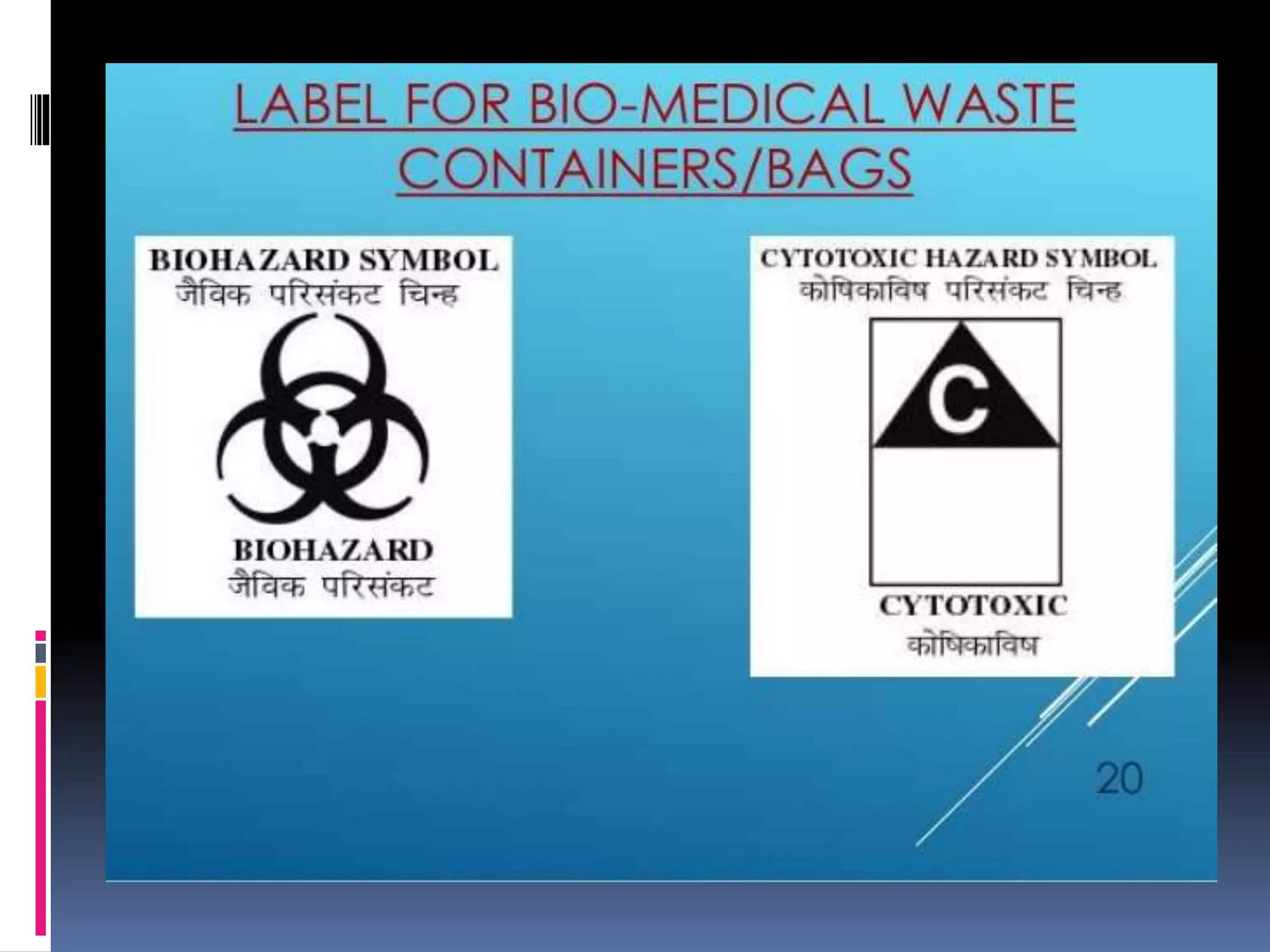
The document discusses biomedical waste management. It defines biomedical waste and outlines the types of waste that are considered biomedical, such as infectious sharps, pathological waste, and chemical waste. It notes that improper management of biomedical waste poses health risks like disease transmission. The document recommends proper segregation, treatment, and disposal of biomedical waste according to the Bio-medical Waste Rules to reduce health and environmental risks. Treatment methods discussed include incineration, disinfection, sterilization, microwaving, and autoclaving. The document emphasizes the importance of safe and responsible management of biomedical waste.