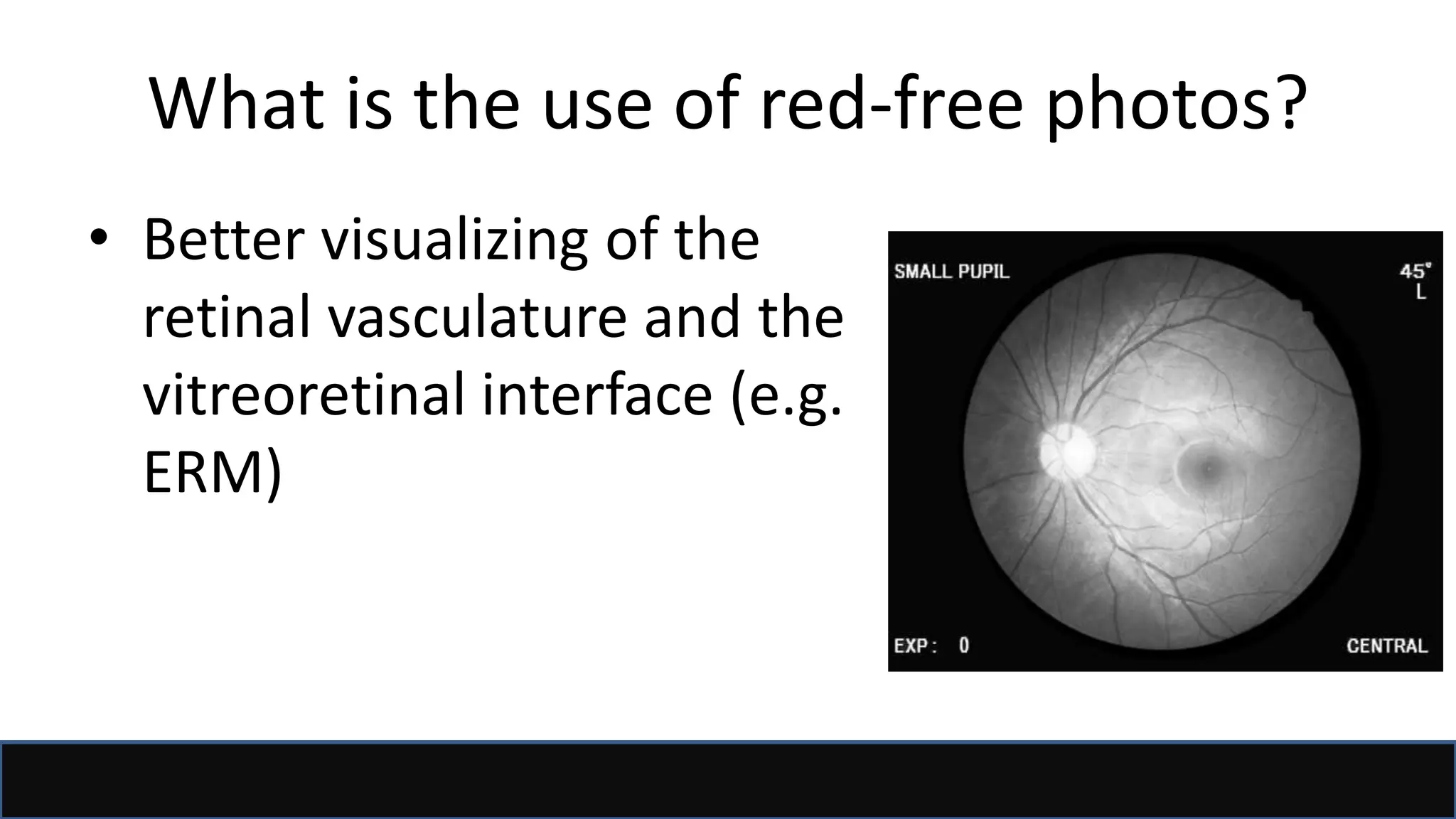
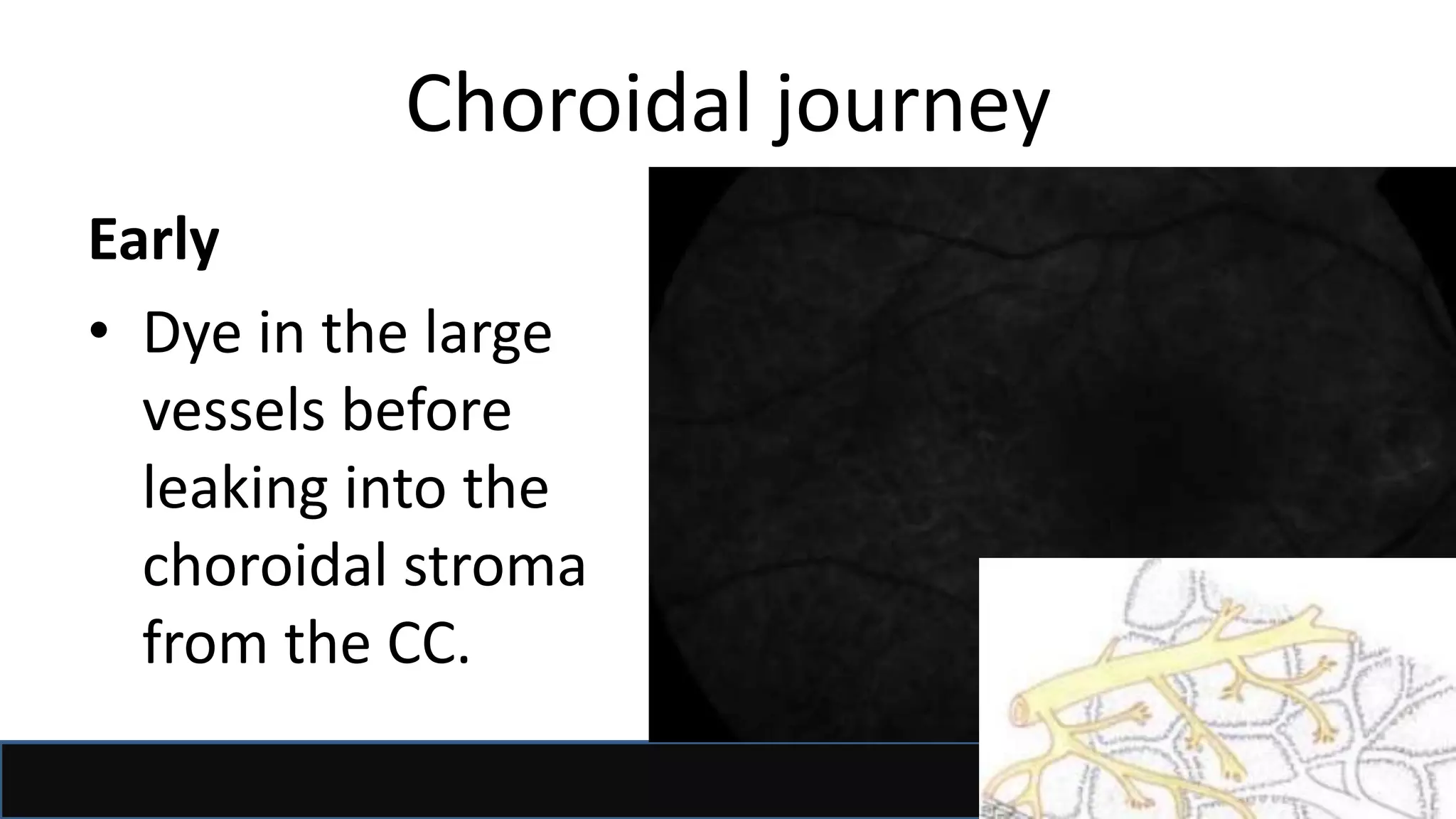
This document provides information about fluorescein angiography (FFA) and indocyanine green angiography (ICGA). It defines FFA as a technique that uses intravenous fluorescein dye to visualize blood flow through retinal, choroidal, and iris tissue. Sodium fluorescein is excited by blue light and emits green light. The document describes the procedures, phases, interpretations, and indications for both FFA and ICGA. It explains that ICGA is better for imaging the choroid since indocyanine green does not leak through choroidal vessels like fluorescein.

![Acknowledgment/References
• Dr Al Yaqdhan Al Ghafri presentation
• Dr Sawsan Nawilaty (AAO 2011)
• AAO BCSC 2015, Retina and vitreous
• Ophthalmology by Yanoff&Dukar
• Retina by Ryan
• Retinal Angiography and Optical Coherence
Tomography (Arevalo [Editor])
• Google!](https://image.slidesharecdn.com/ffaicg-170916141405/75/fundus-fluorescein-and-indocyanine-green-angiography-2-2048.jpg)