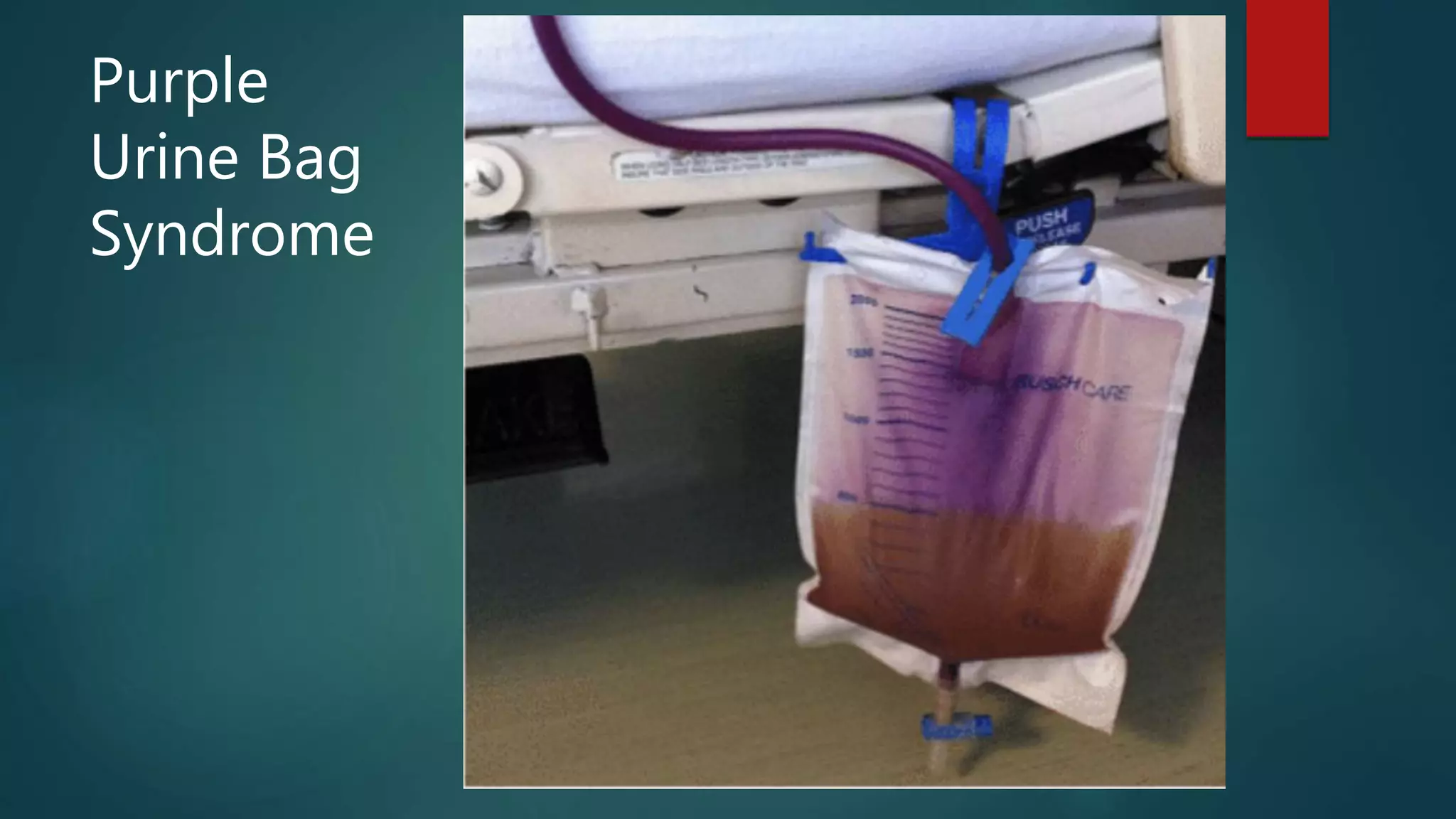
The document summarizes a tele-continuing nurse education session on the topic of intermittent catheterization (IMC) versus indwelling catheterization (IDC) for management of urinary incontinence and retention. It provides objectives and definitions of incontinence and retention. Guidelines are given for when IMC is and is not appropriate, along with requisites, general guidelines on frequency of catheterization based on bladder scan results, and nursing care plans for patients on IDC or post-catheterization. Potential issues like purple urine bag syndrome are also mentioned.