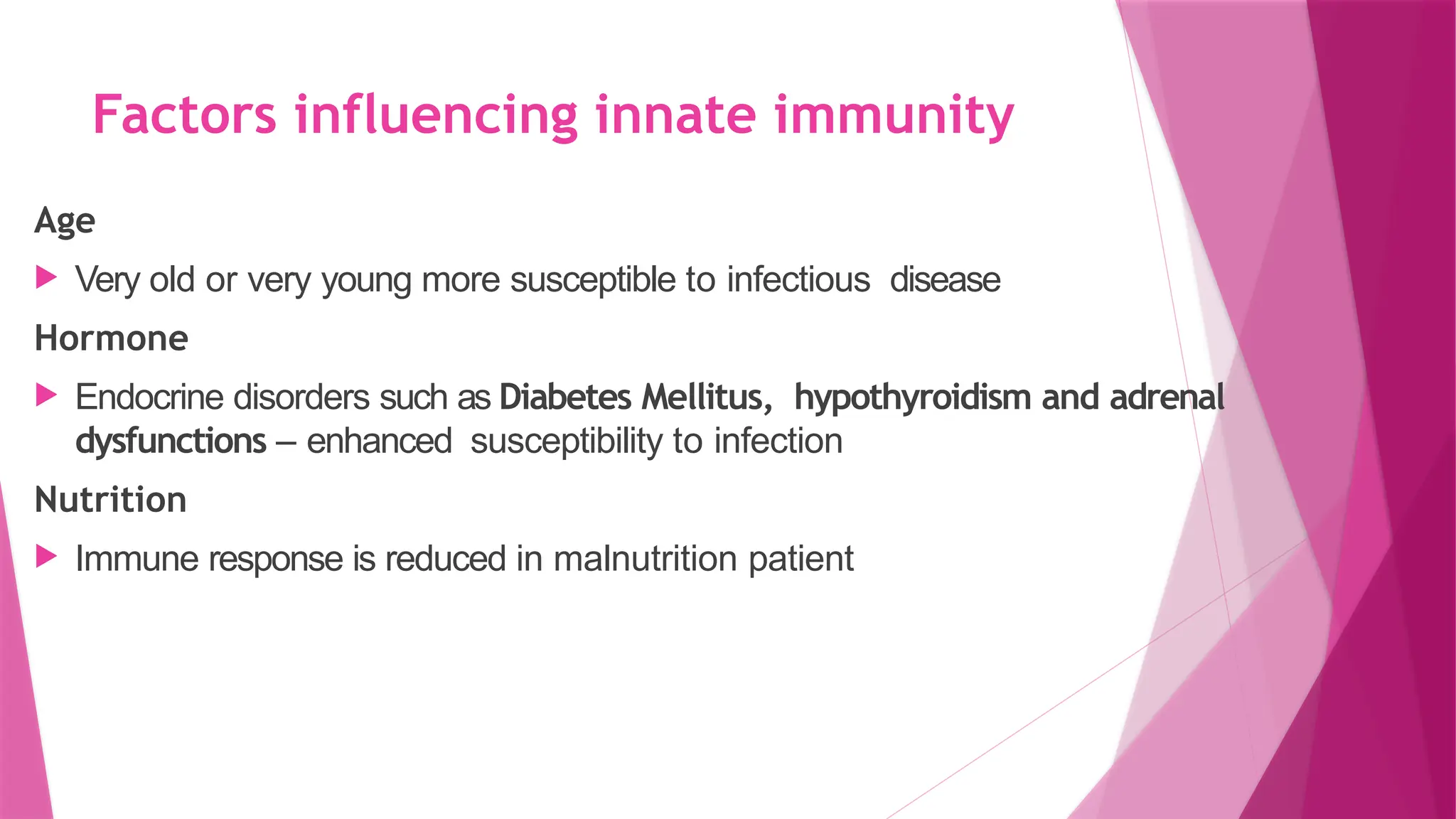
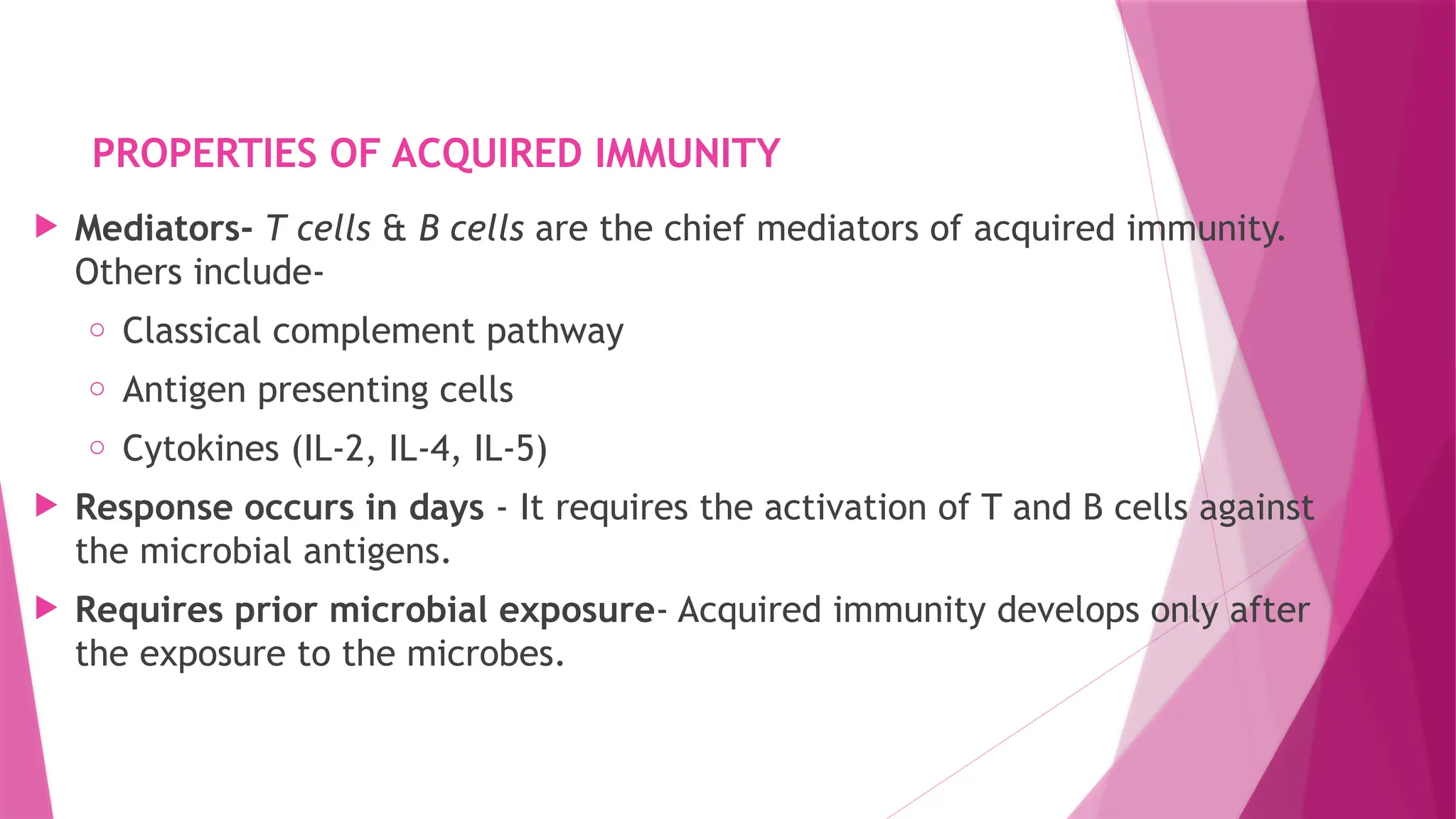
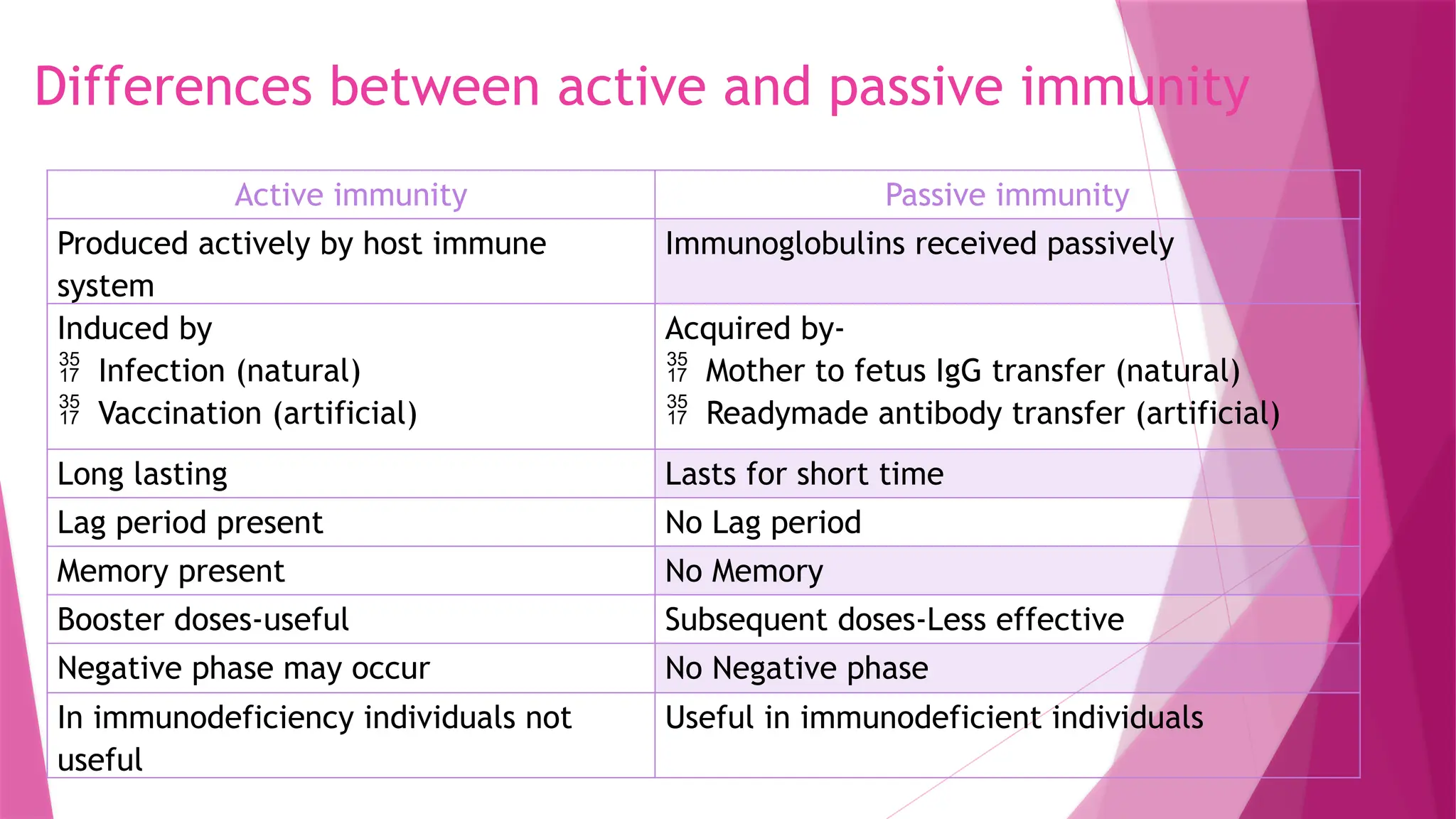
The document provides an overview of immunity, distinguishing between innate and acquired immunity, their components, and mechanisms. Innate immunity, which is present from birth, acts quickly and is non-specific, while acquired immunity develops over time, is specific, and involves memory. The text details various cells, responses, and interactions that characterize both types of immunity and highlights the importance of bridges between these two systems.