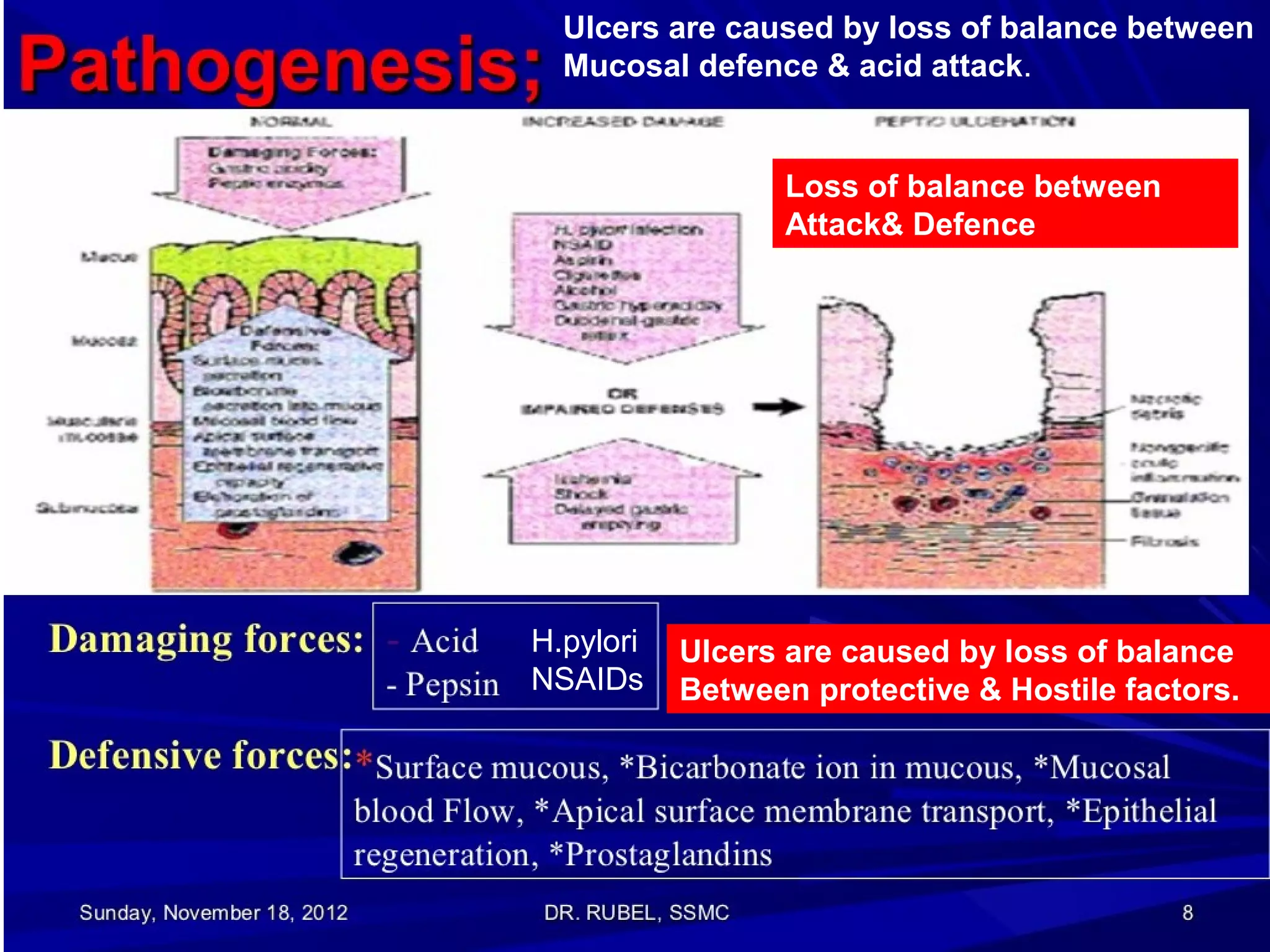
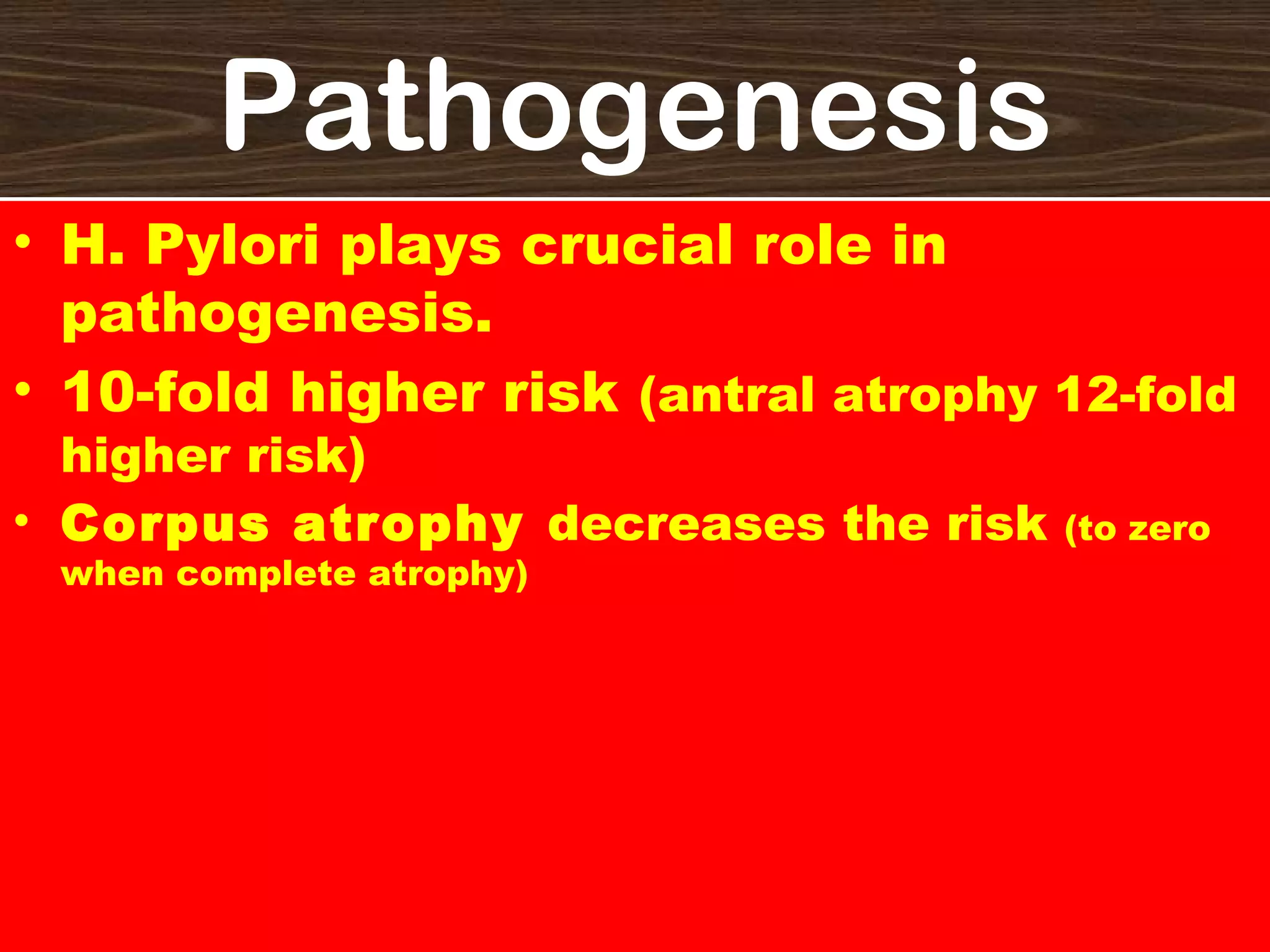
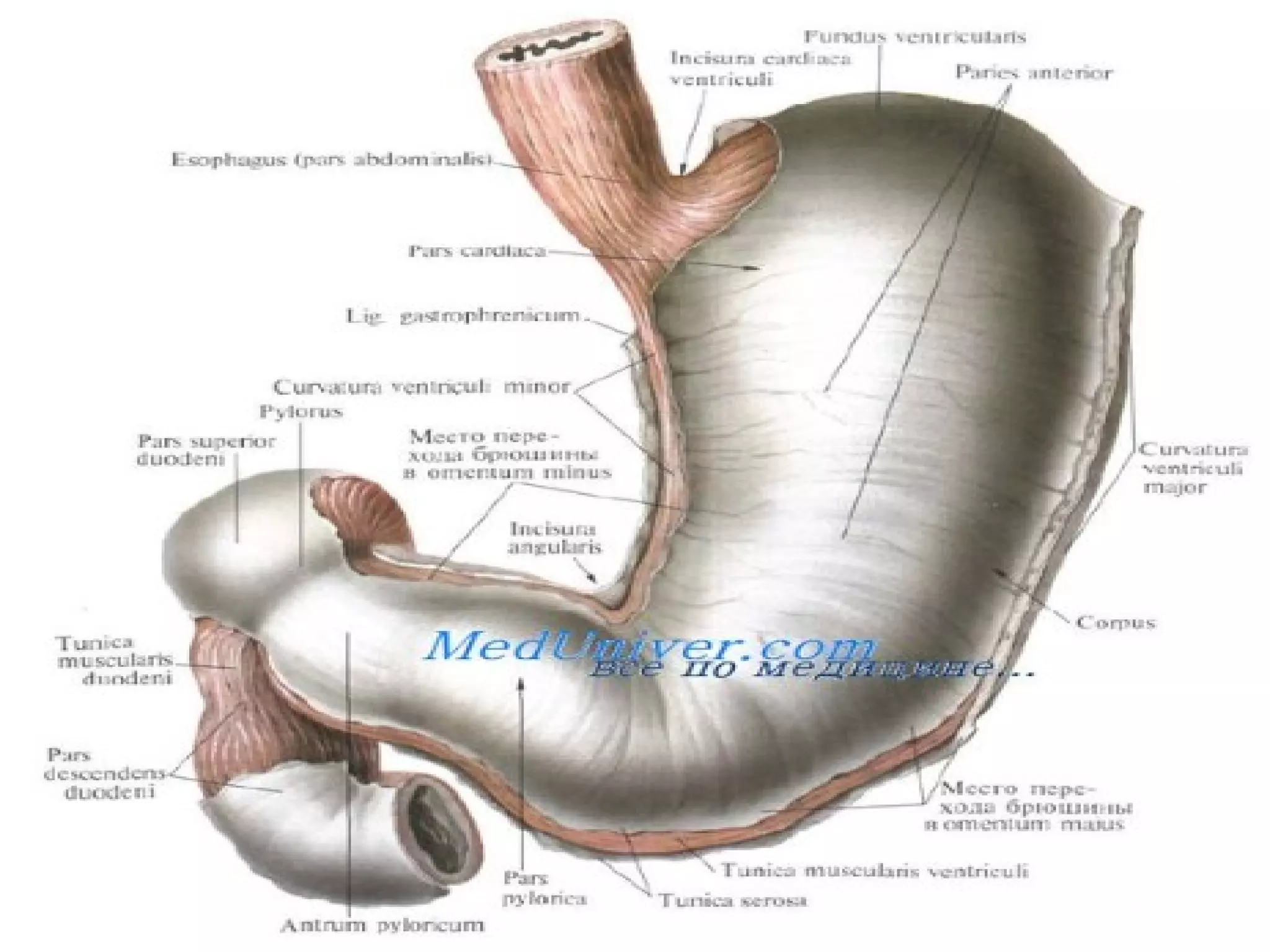
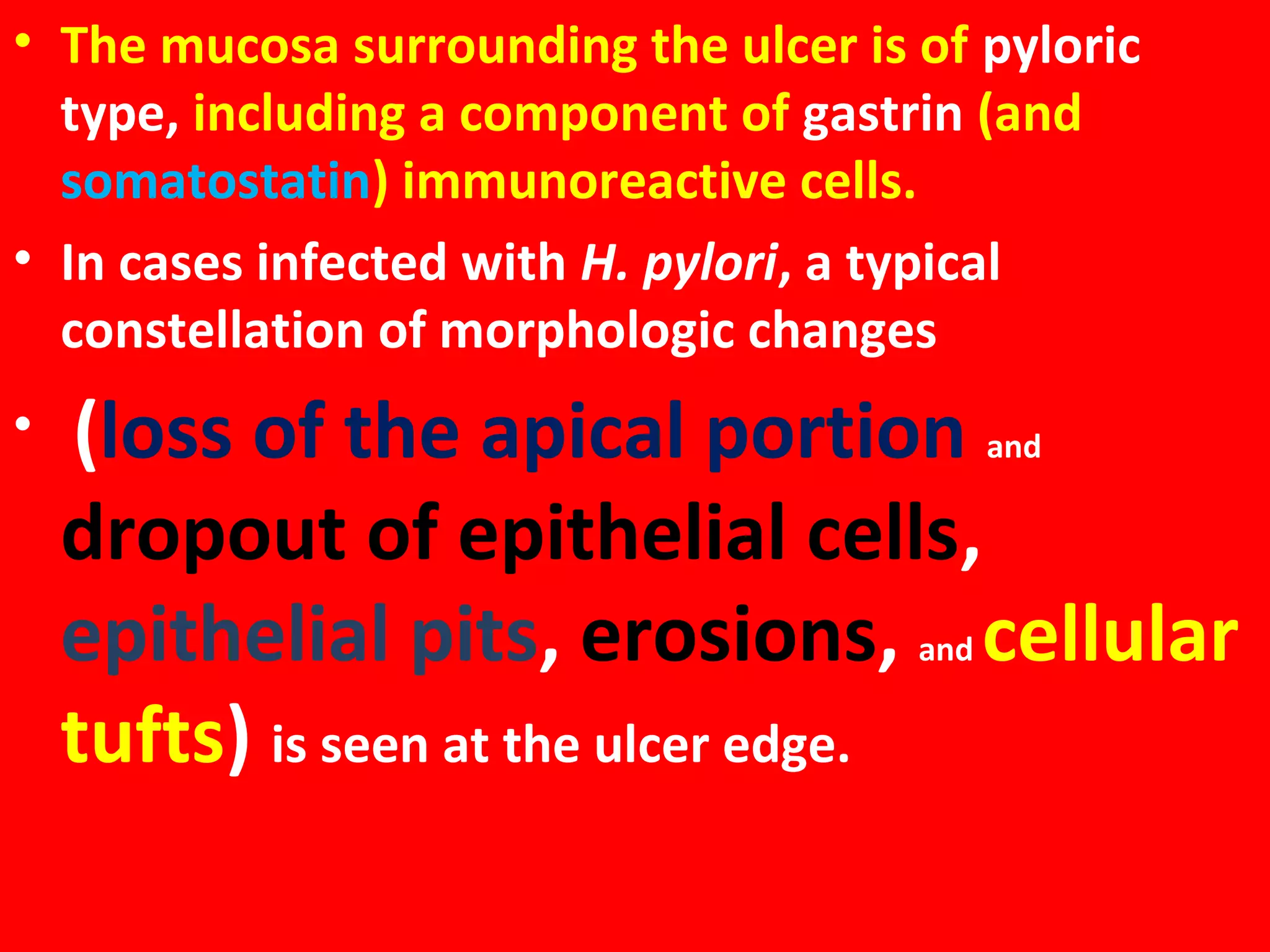
H. pylori plays a crucial role in the pathogenesis of peptic ulcers. It has been found in 90% of patients with chronic gastritis, 95% with duodenal ulcer disease, and 70% with gastric ulcer. Peptic ulcers are caused by a loss of balance between protective and hostile factors in the stomach and duodenum. Factors like H. pylori infection, NSAIDs, and excess acid secretion can damage the mucosal lining, while factors like mucus, bicarbonate, and blood flow work to protect it. Chronic peptic ulcers form in areas of the stomach and duodenum with reduced acid levels. They appear as round or oval lesions that penetrate