After completing this lesson, you will be able to:
Encourage active participation by the patient in decision-making and explain choices or rights to the patient in a patient-centered manner
Assess patient desire and capacity to be involved and responsible in the decision-making process
Determine patient preferences and priorities for treatment
Identify strategies to assist patients in discussing preferences and priorities with clinician
Support the patient in the decision-making process in alignment with desired level of engagement
Describe a treatment plan
Assess barriers to patient adherence to the plan
Develop a plan with the patient for addressing adherence challenges
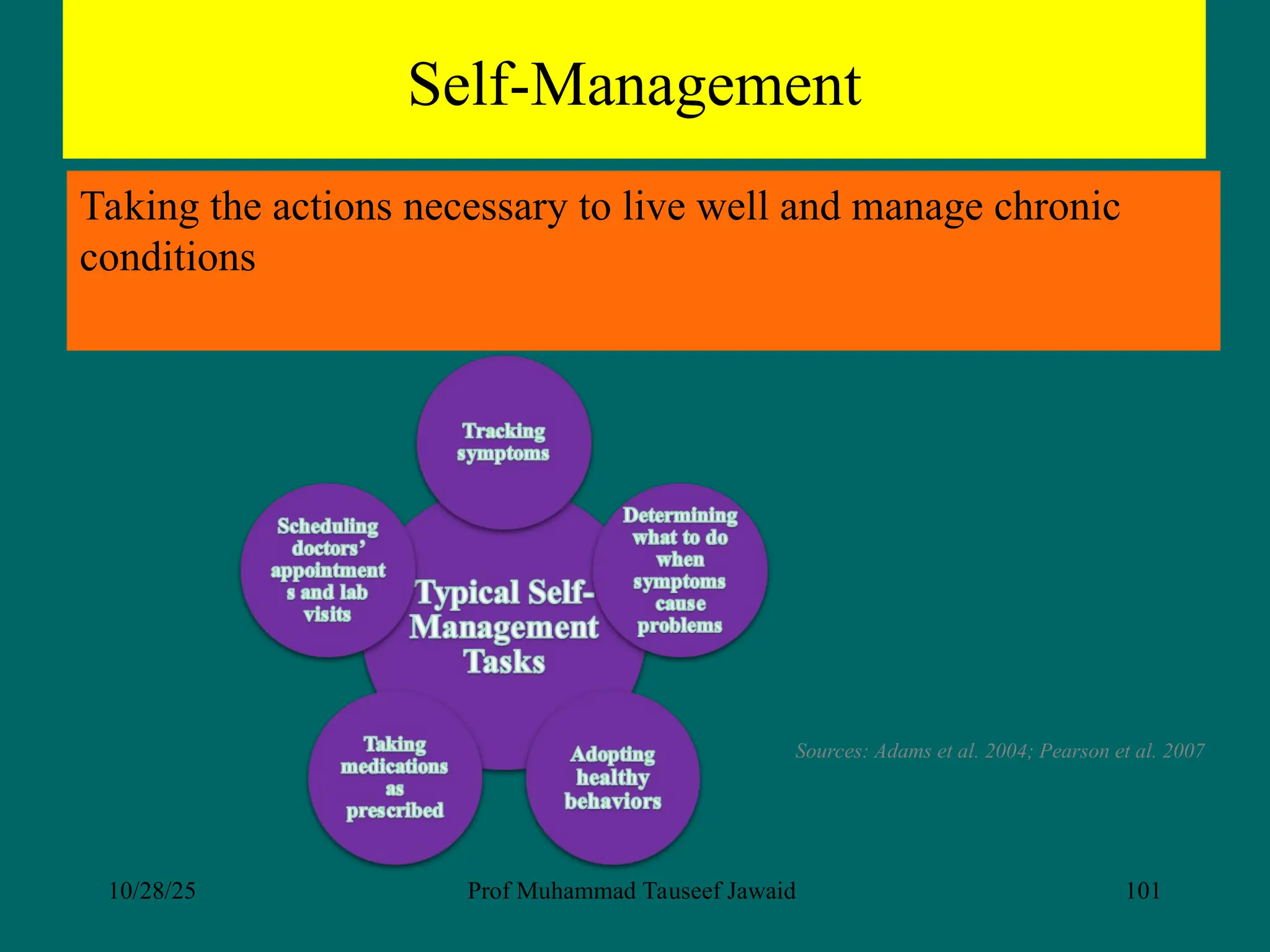
Identify self-management and health promotion resources














































































































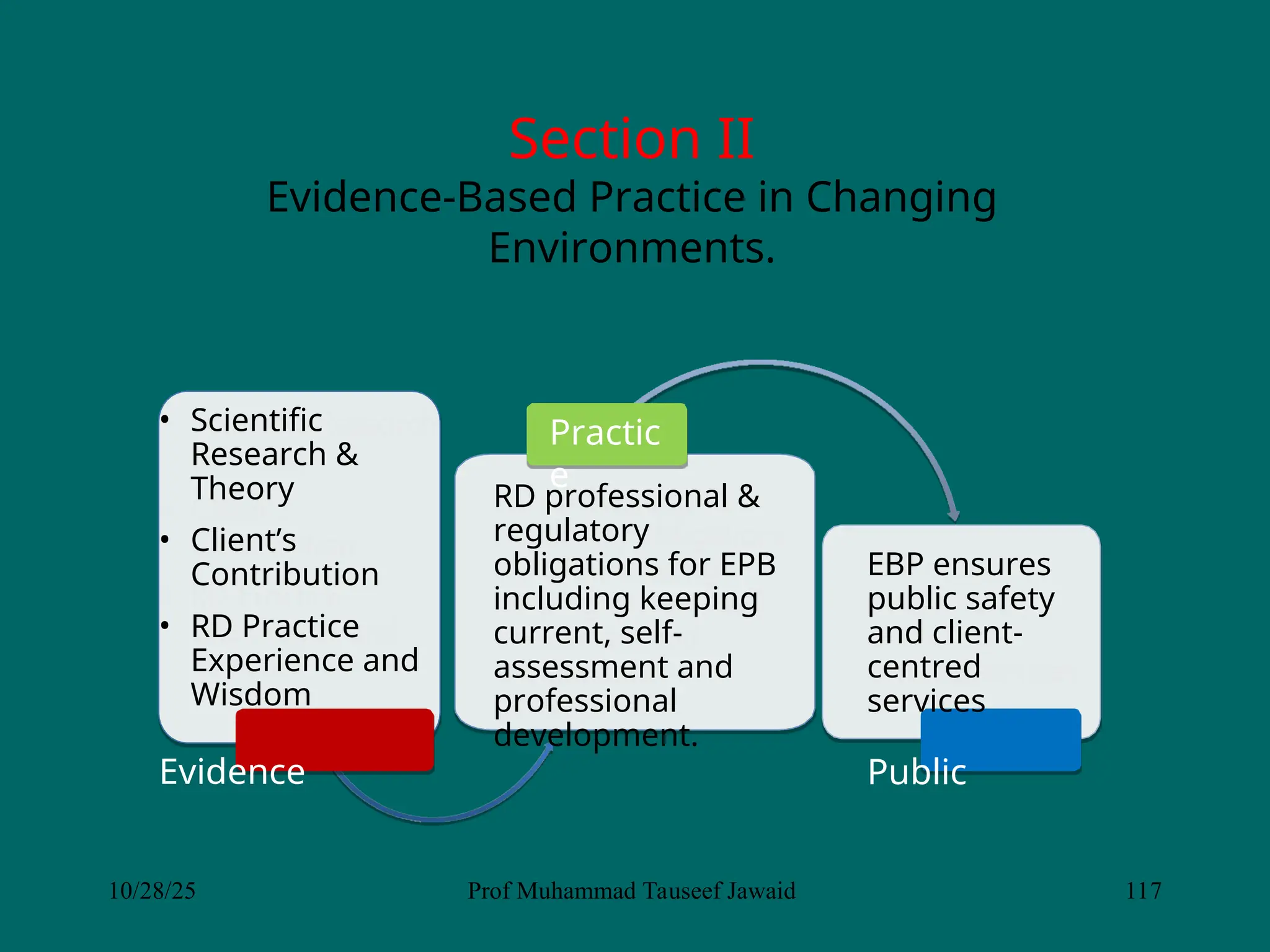
![“Evidence-based decision-making
refers to making decisions that affect
[client] patient care based on the best
available evidence”
10/28/25 Prof Muhammad Tauseef Jawaid 114](https://image.slidesharecdn.com/lectureconceptofhealthshareddecisionmaking2025-251028042501-7052fb6f/75/Lecture-Concept-of-Health-Health-Literacy-and-Shared-decision-making-2025-ppt-114-2048.jpg)