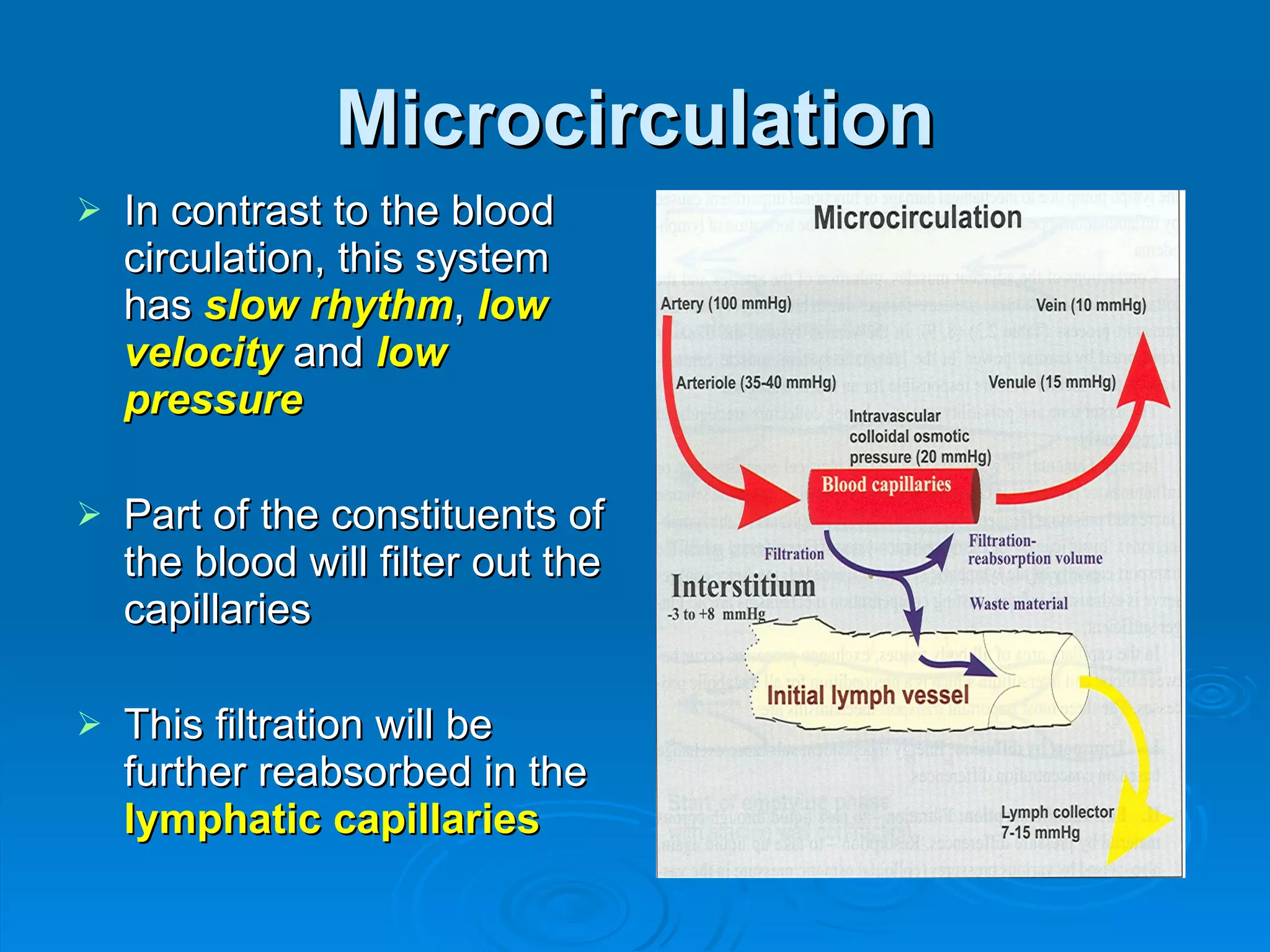
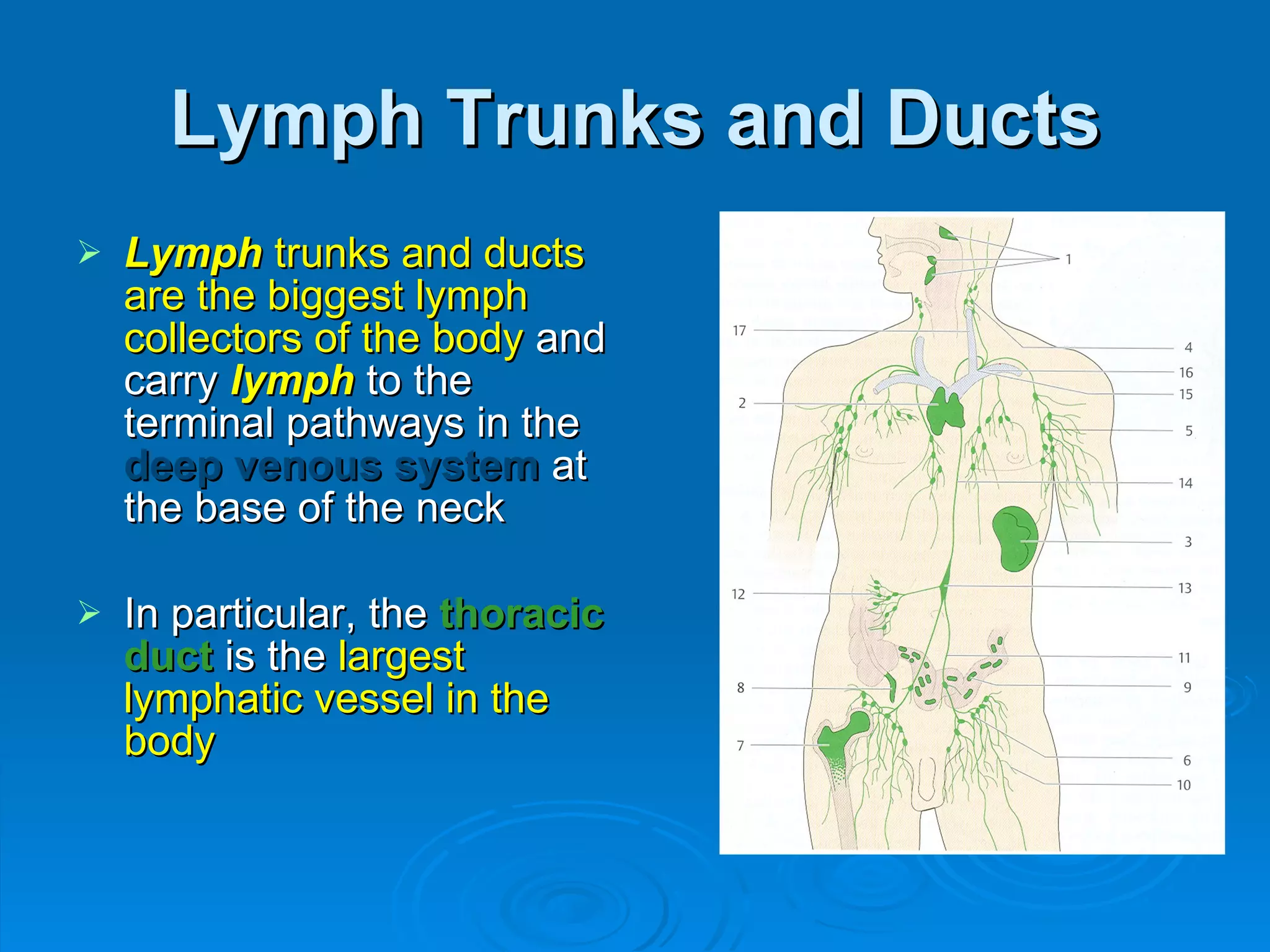
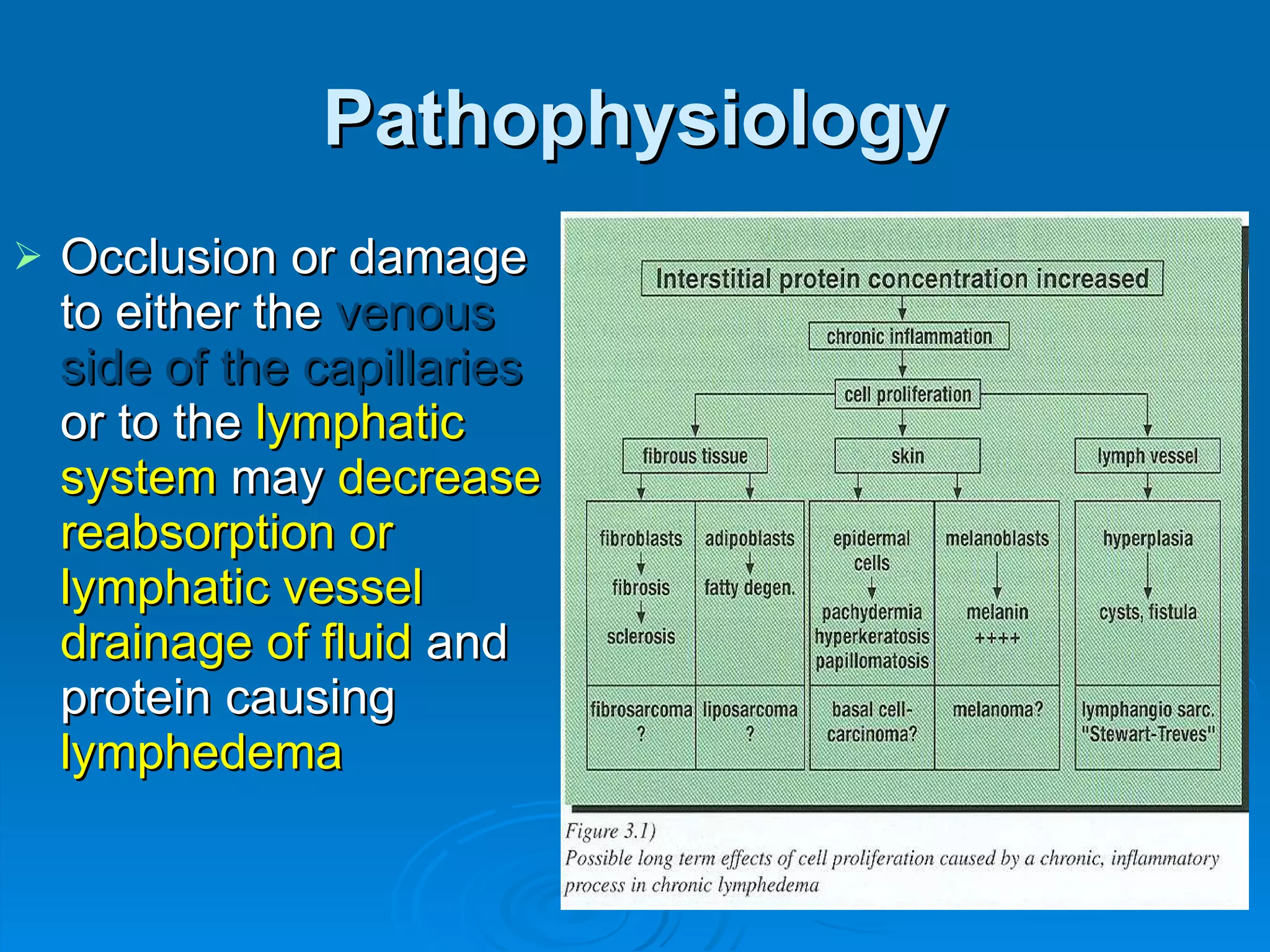
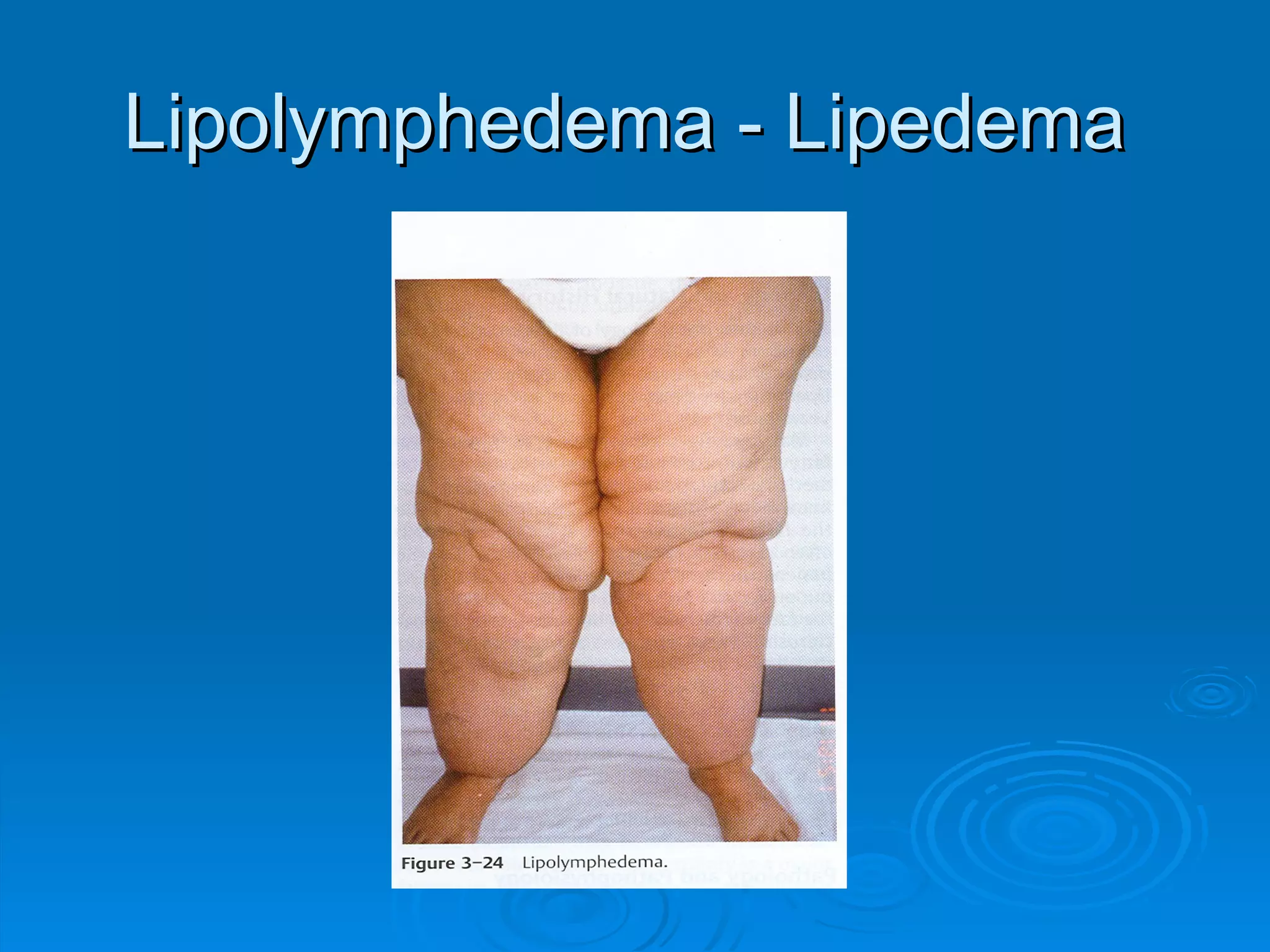
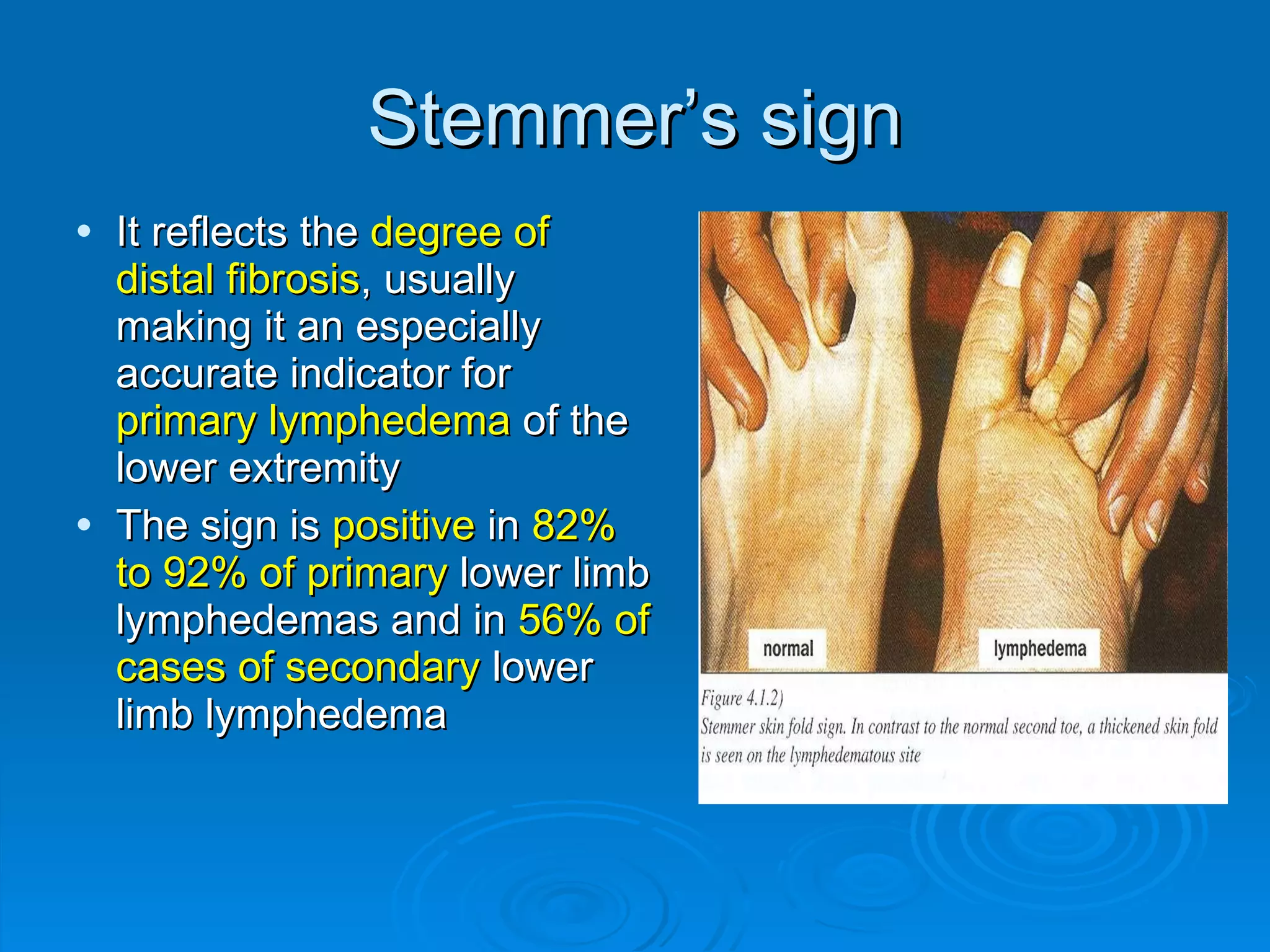
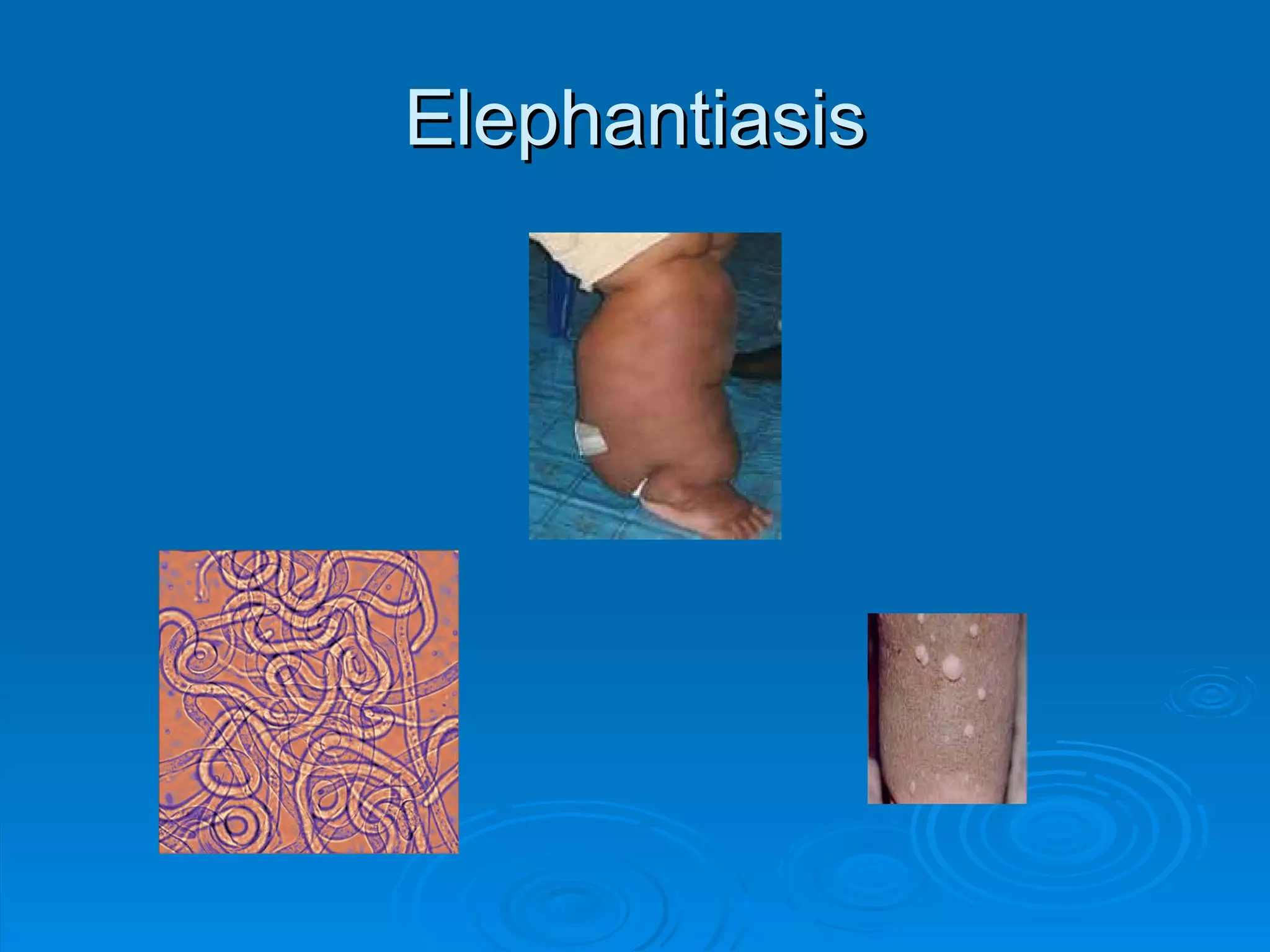
The document provides a comprehensive overview of lymphedema, detailing the anatomy and physiology of the lymphatic system, causes of lymphedema (both primary and secondary), its clinical presentation, and management options. It emphasizes the importance of lymphatic circulation in fluid balance and outlines various diagnostic tools and stages of lymphedema. Additionally, the document discusses complications and contraindications for treatment, particularly emphasizing the need for proper care in patients with concurrent medical conditions.