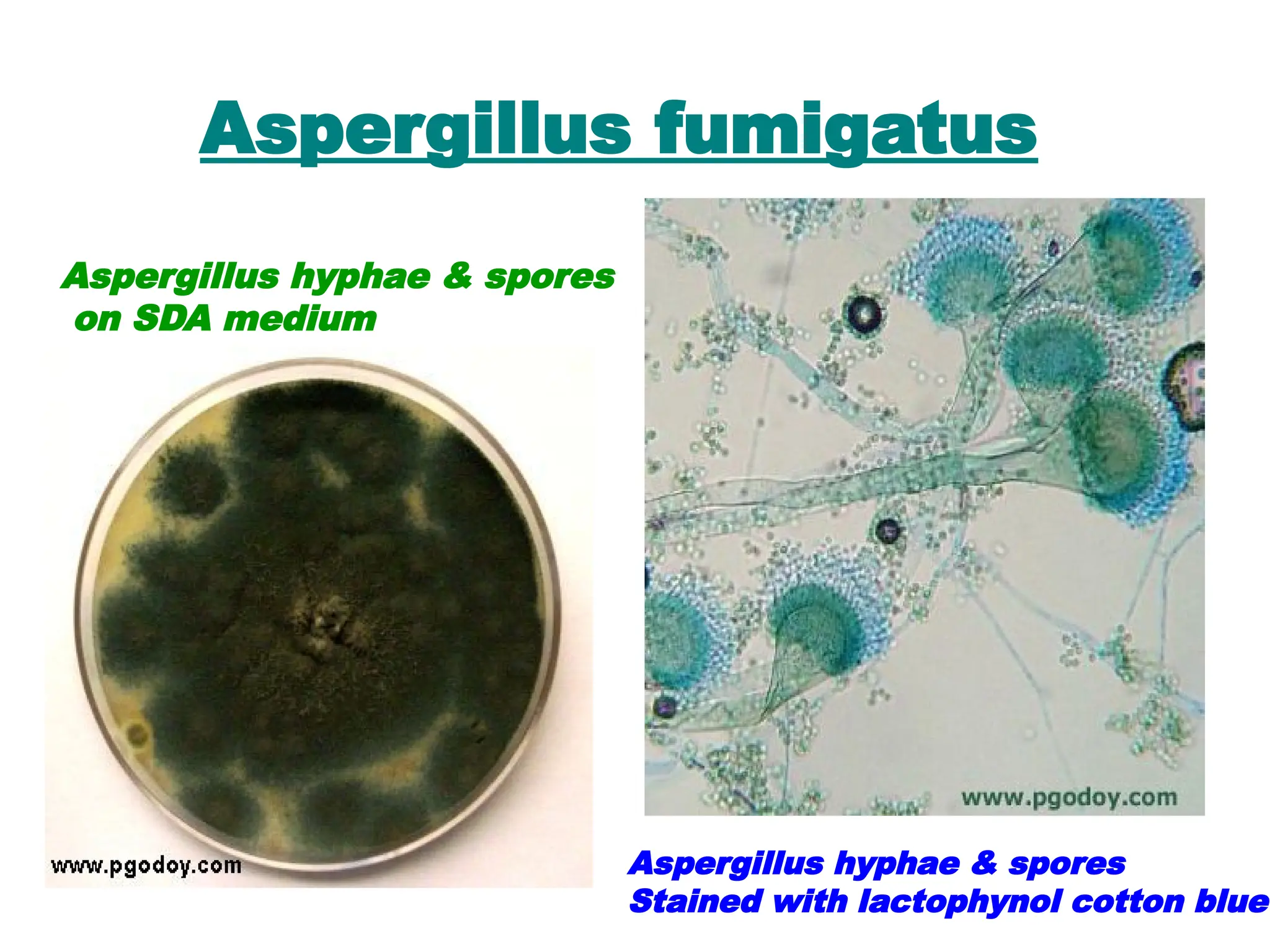
The document discusses opportunistic infections (OIs), which occur when the immune system is compromised, leading to increased susceptibility to various pathogens, especially in immunocompromised patients, such as those with AIDS, cancer, or undergoing transplant procedures. It details the types of immune deficits, associated infections, risk factors, and specific opportunistic pathogens, such as bacteria, viruses, and fungi, as well as their laboratory diagnosis methods. Additionally, it highlights the challenges in managing these infections due to the complexity of the host's immune response and the nature of the opportunistic organisms.