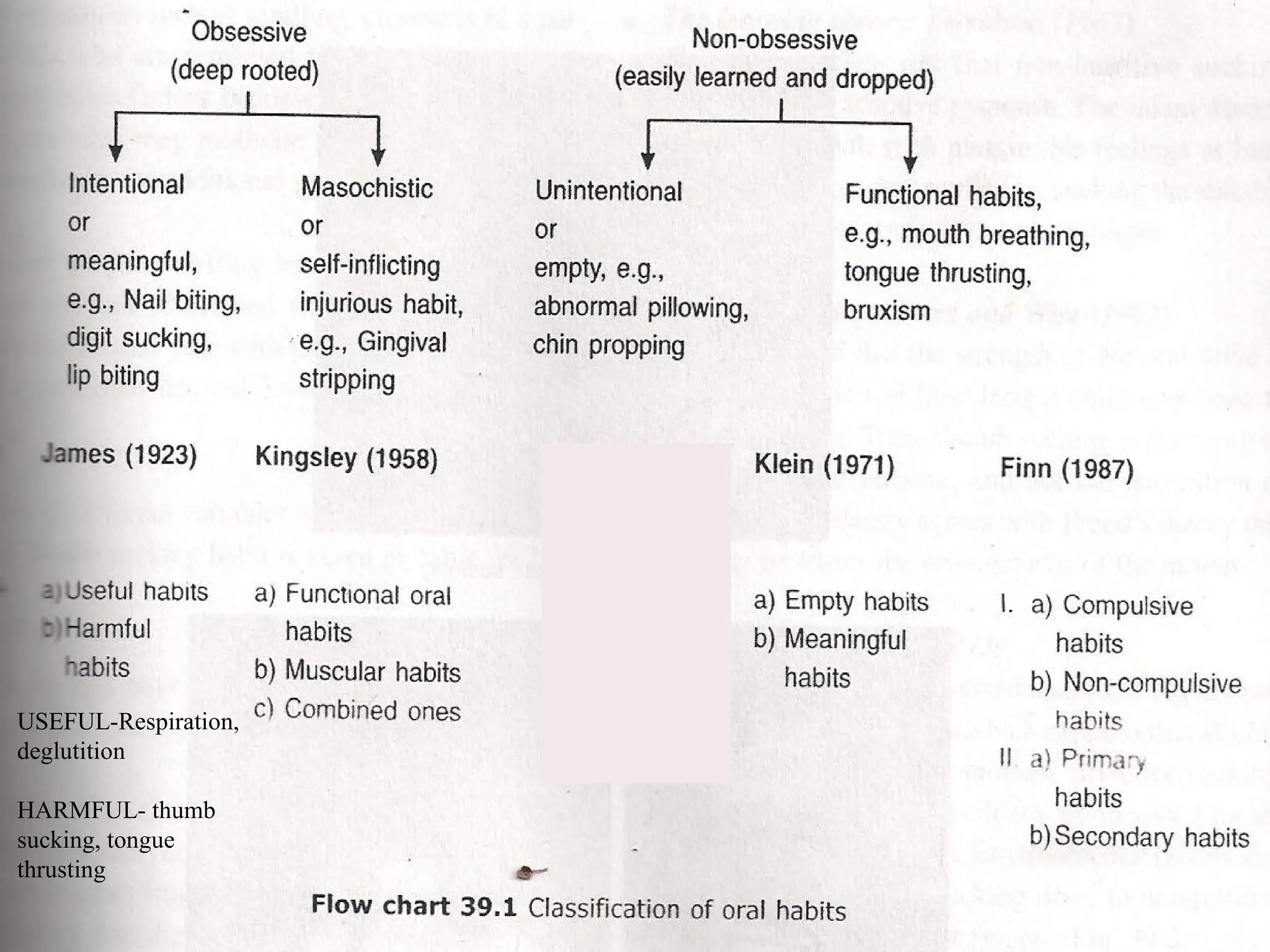
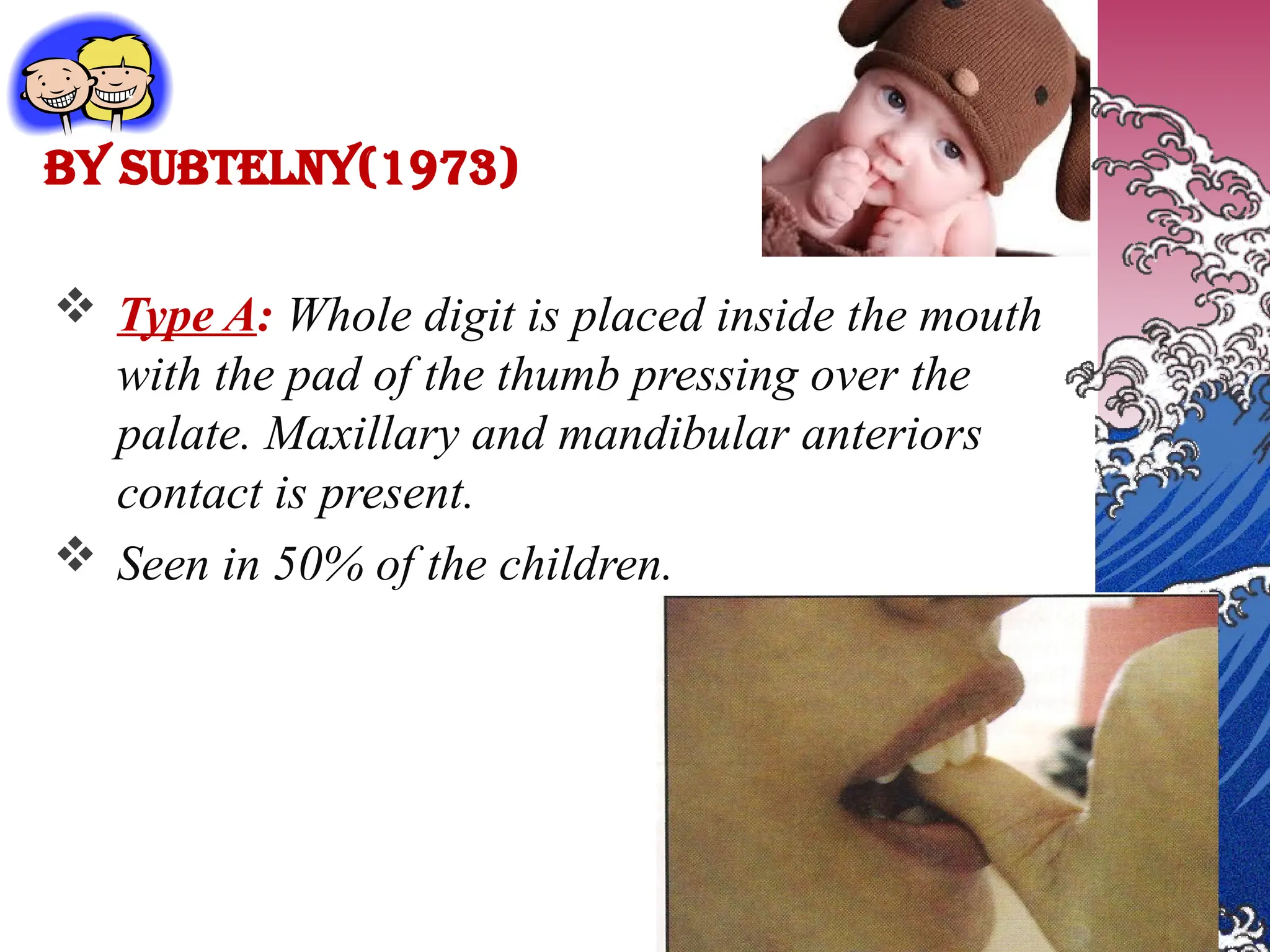
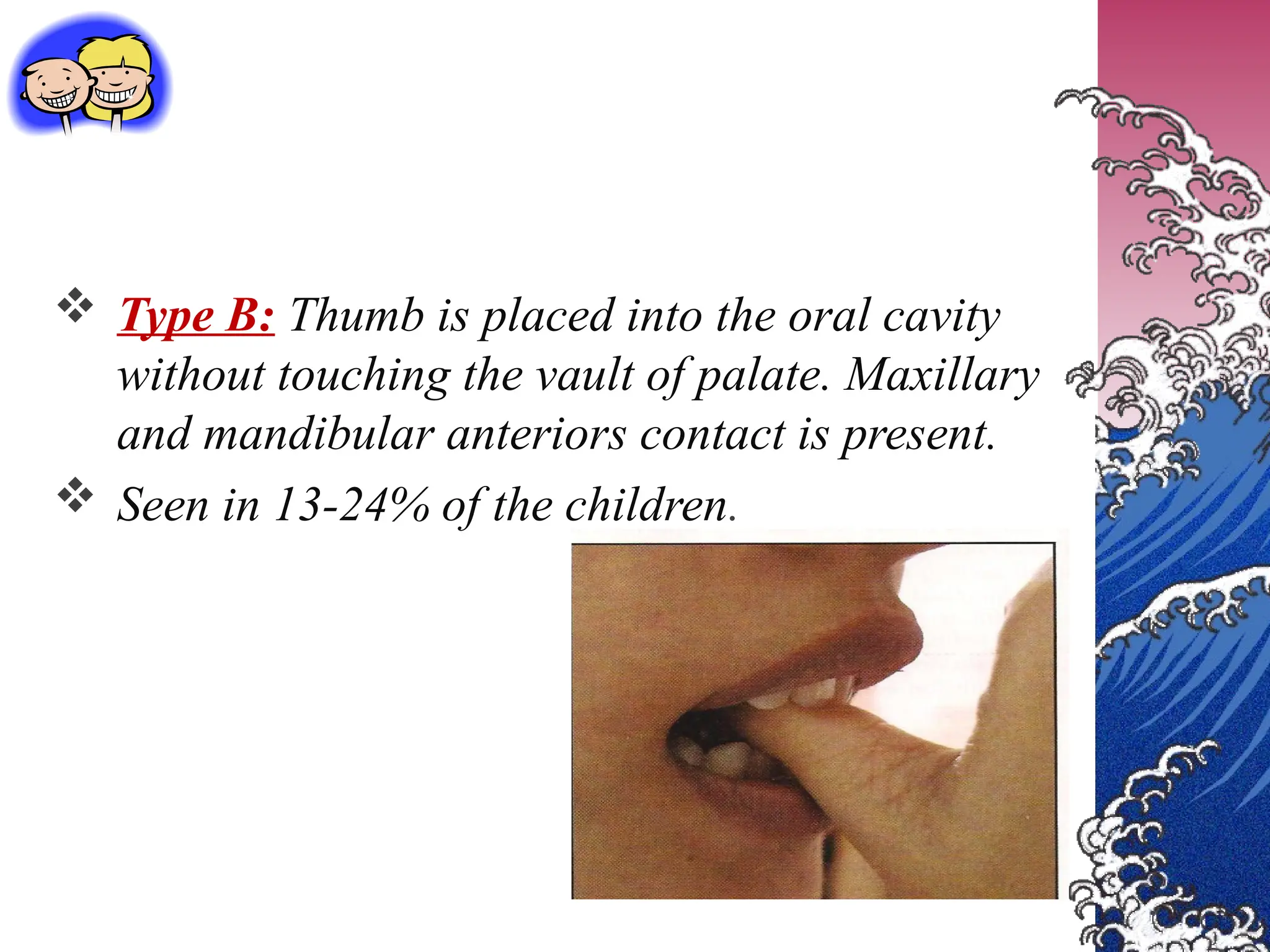
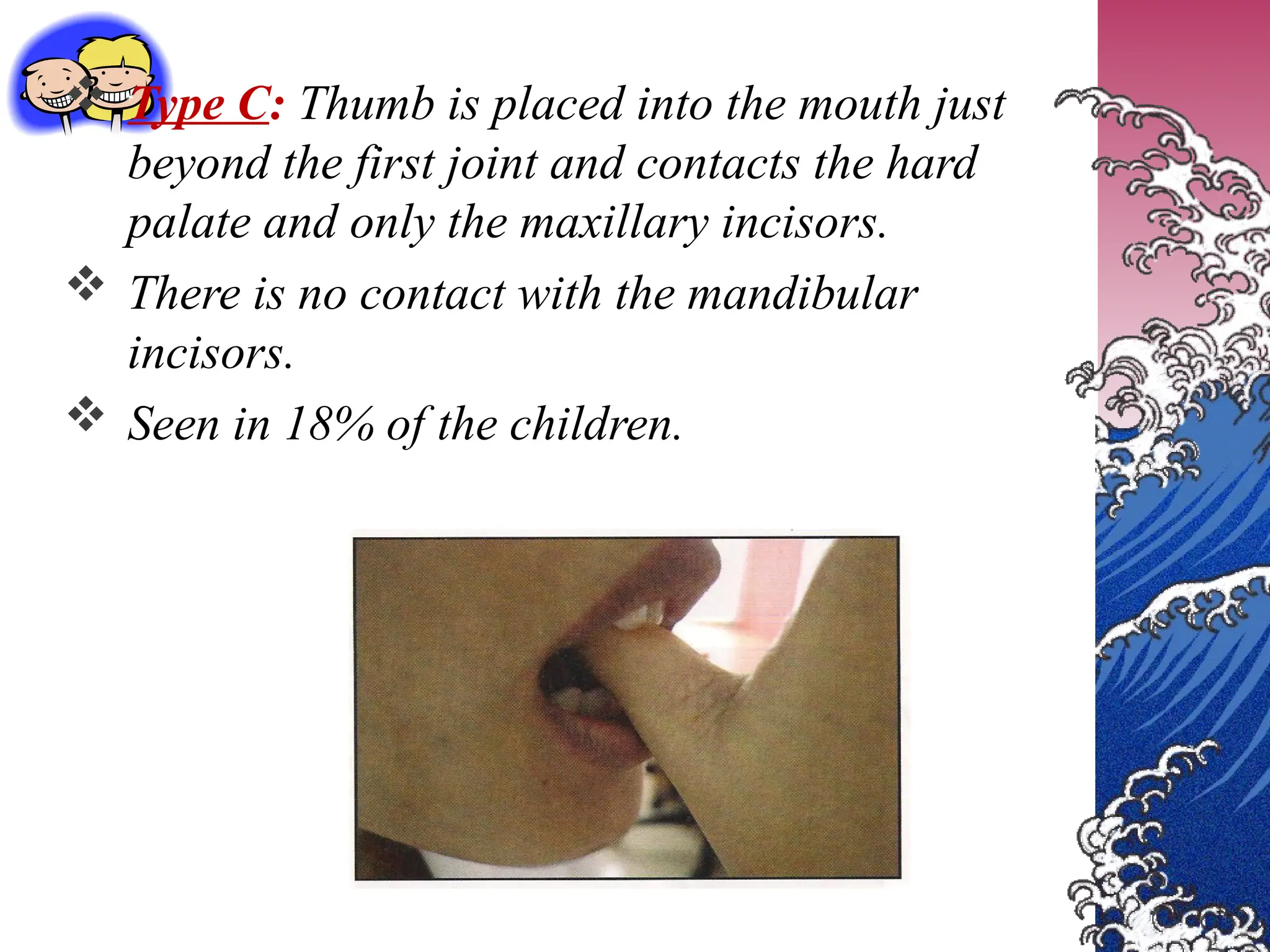
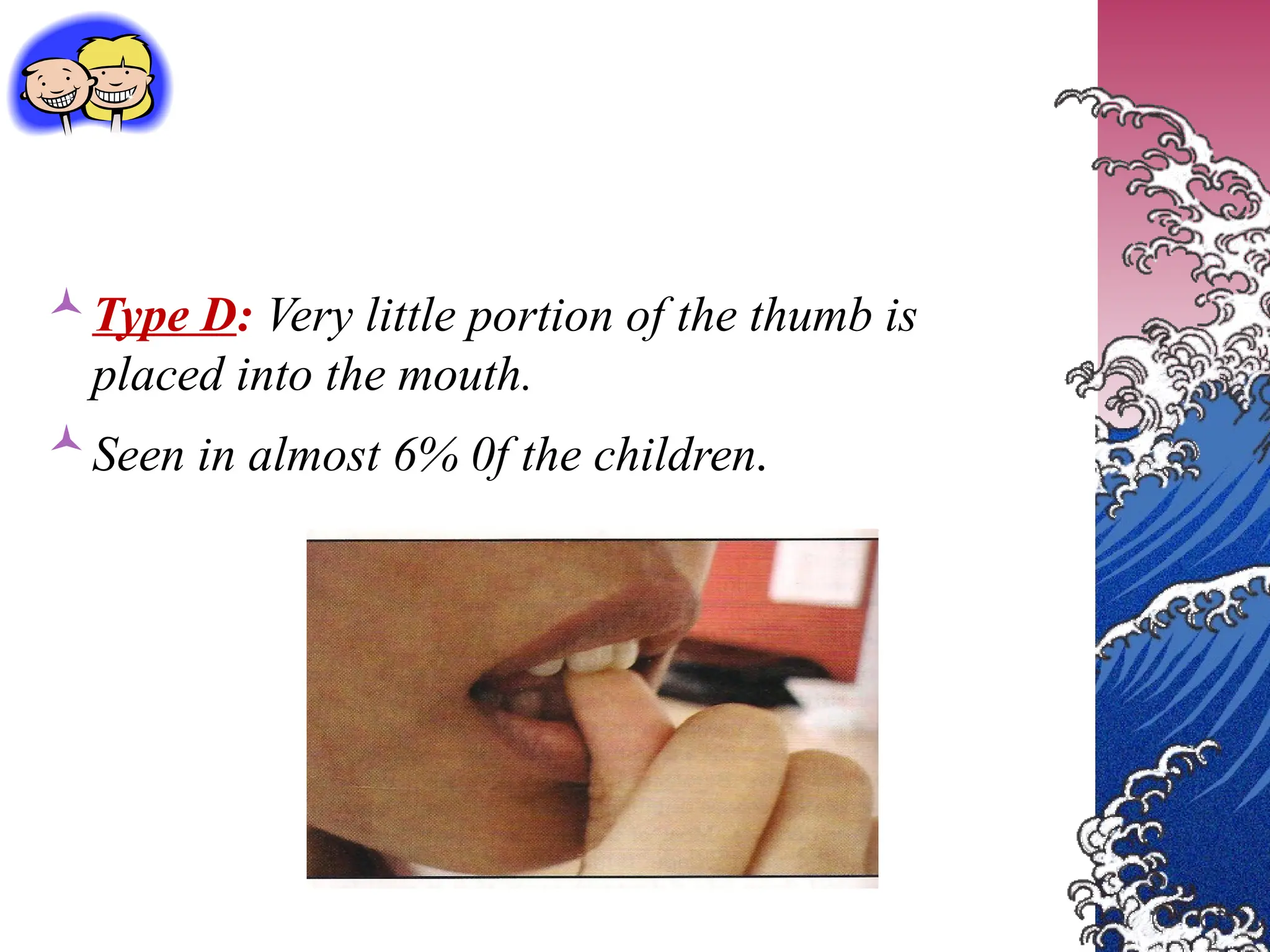
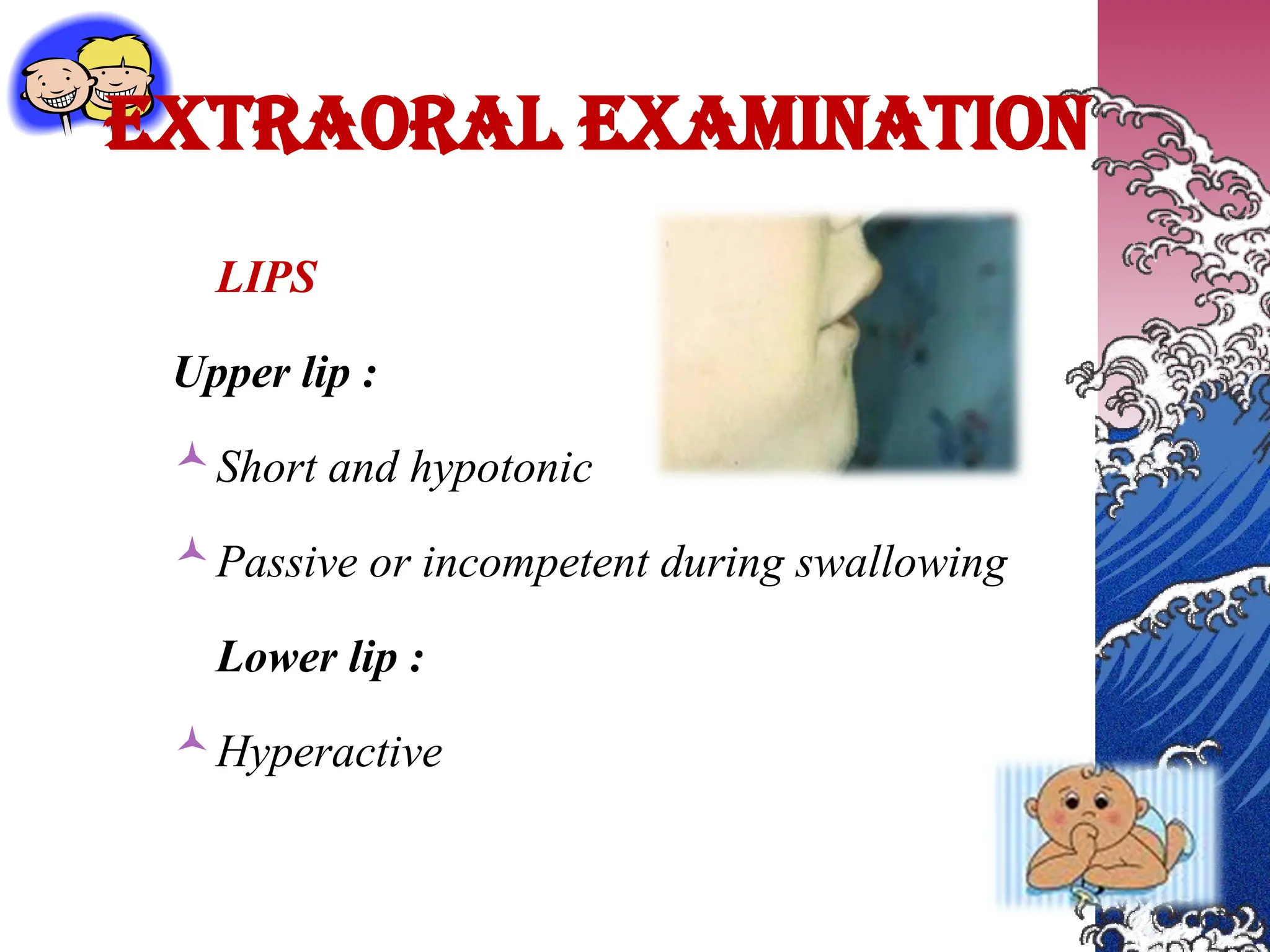
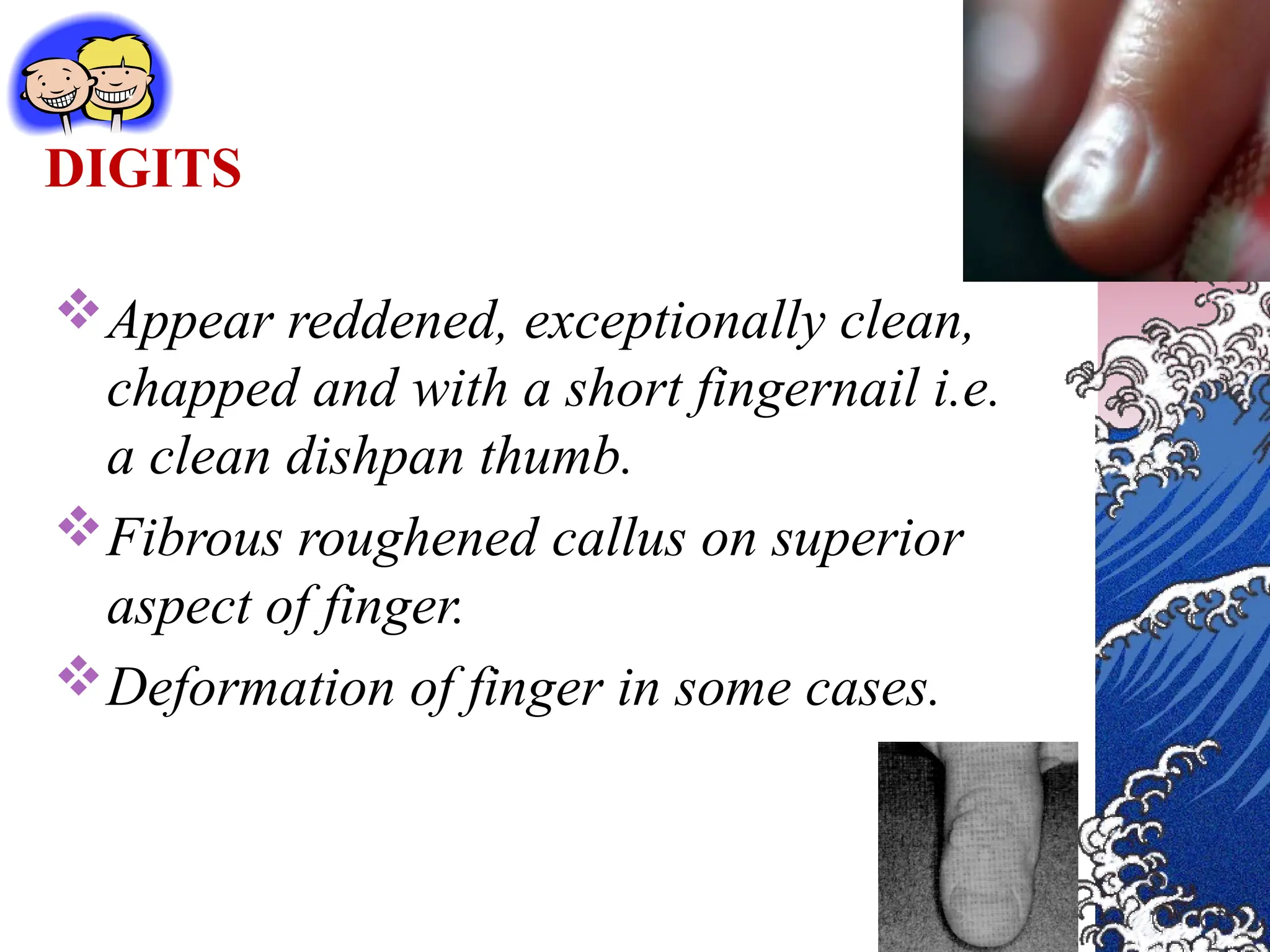
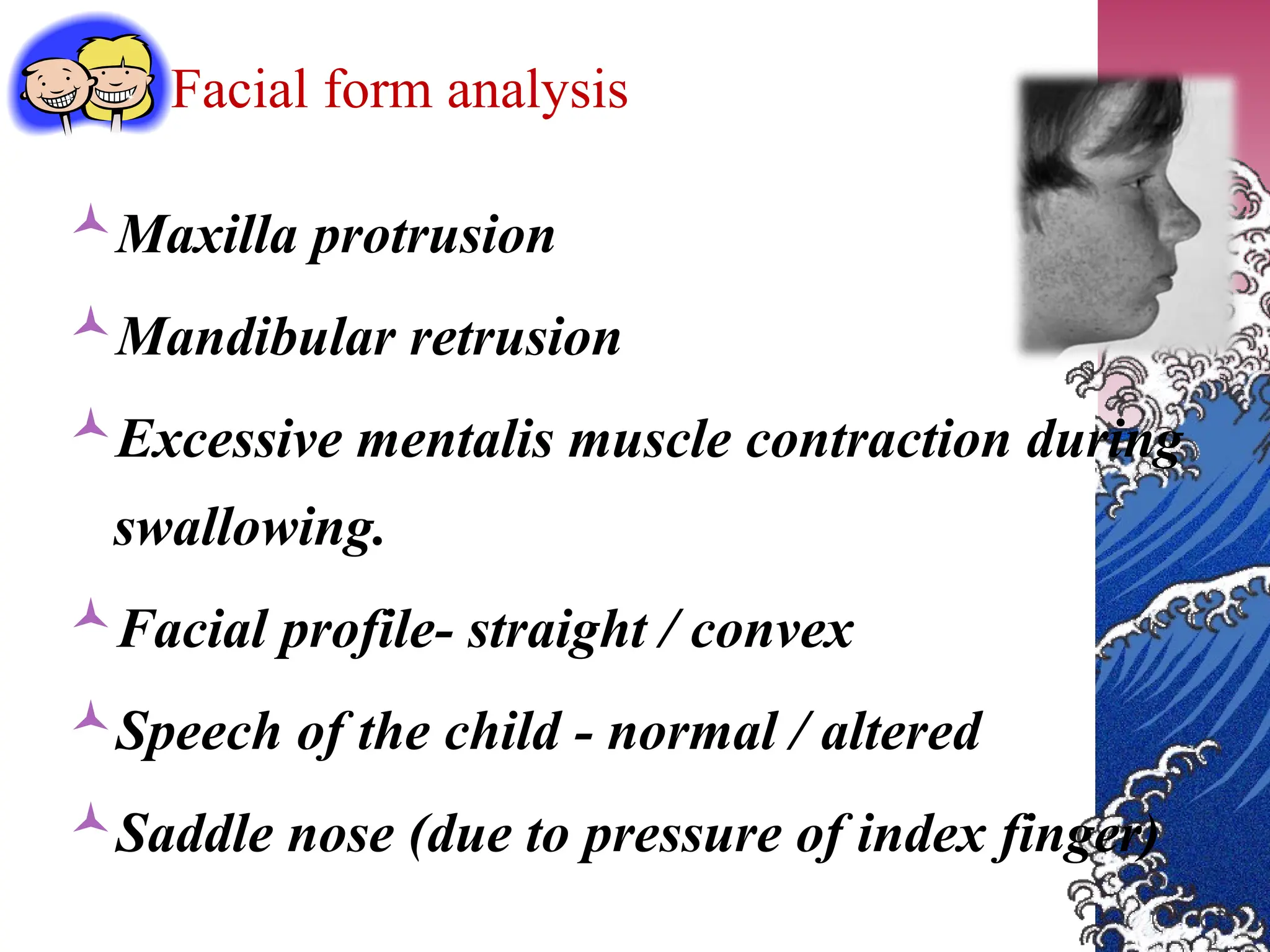
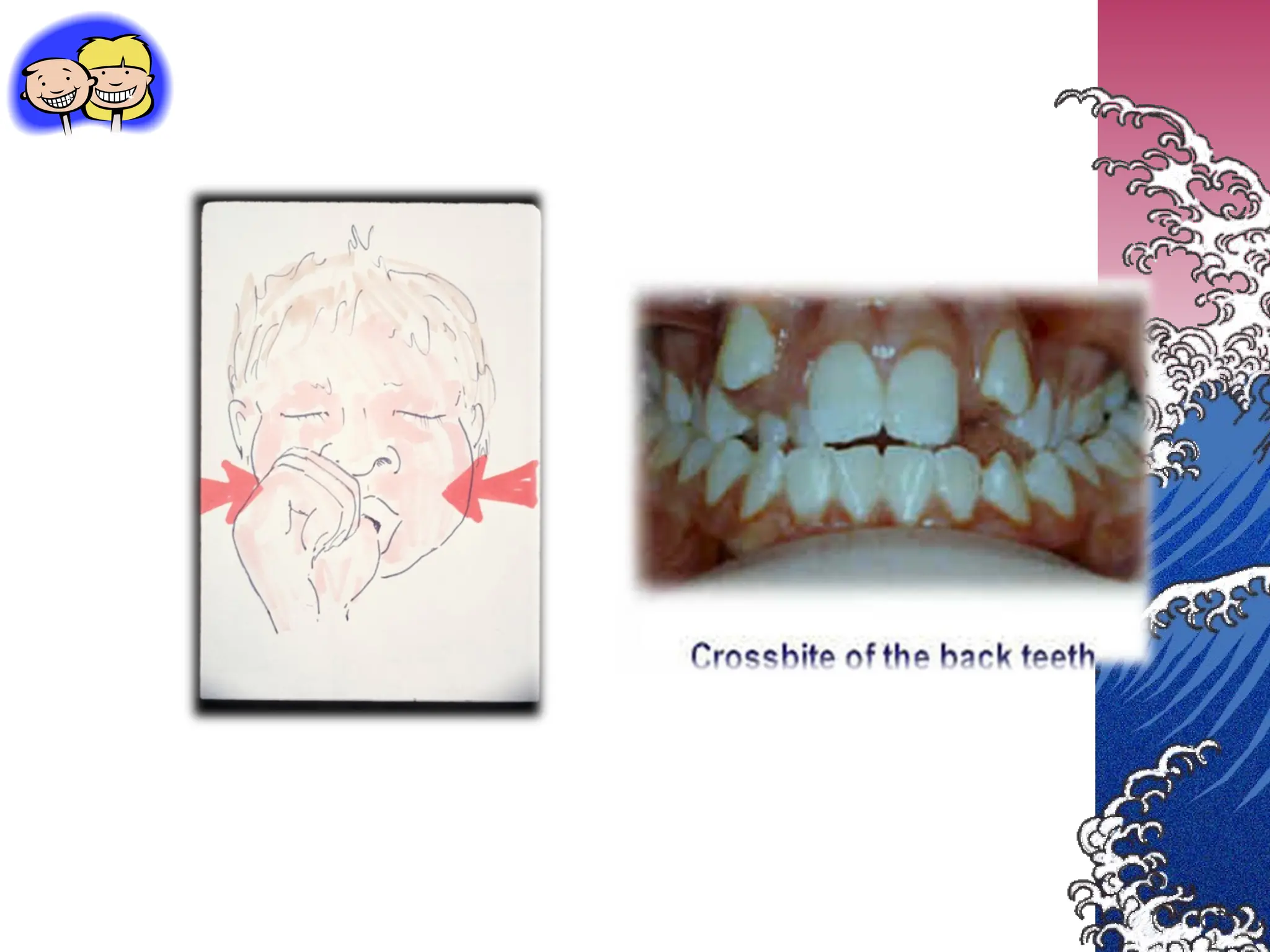
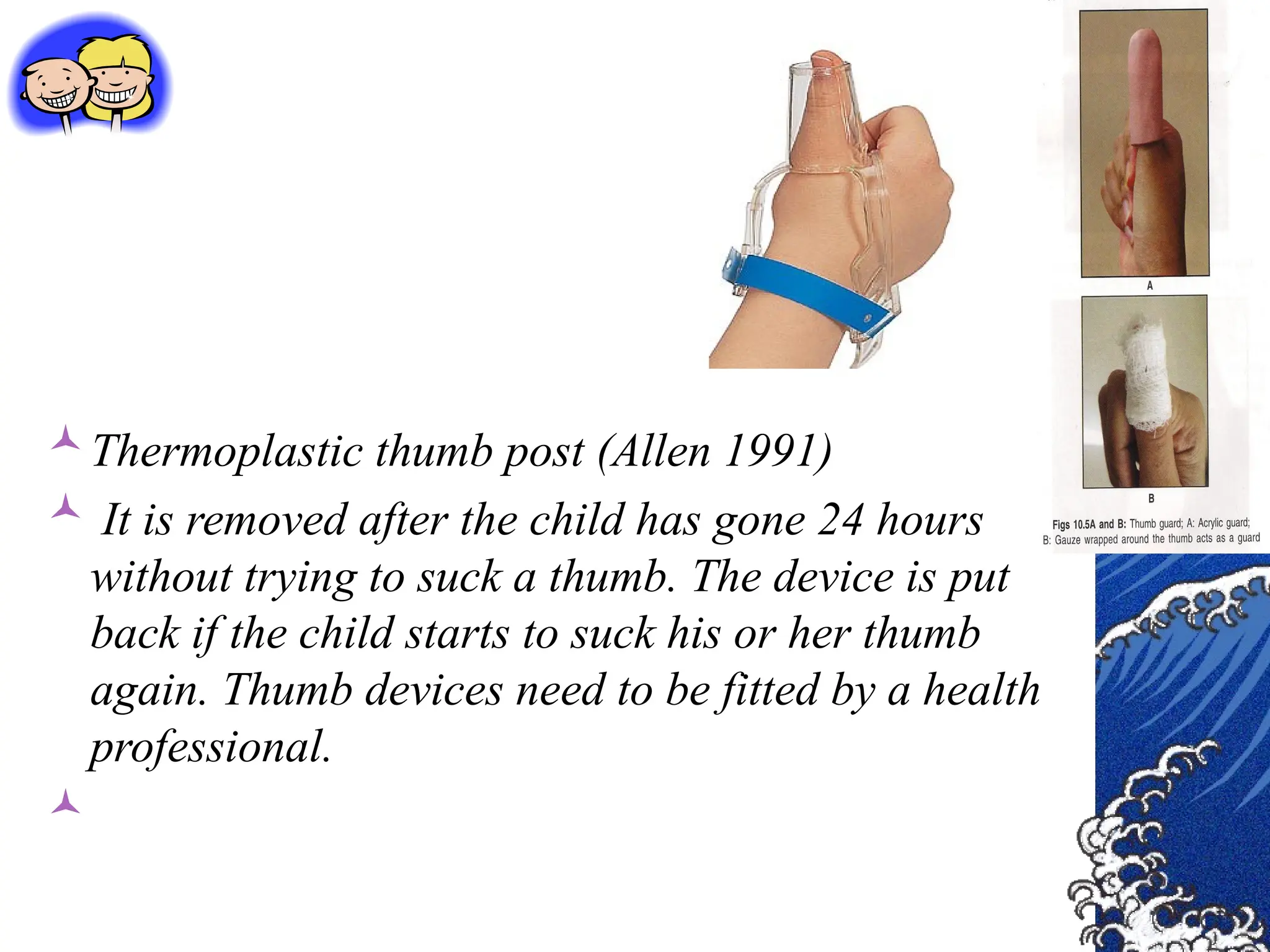
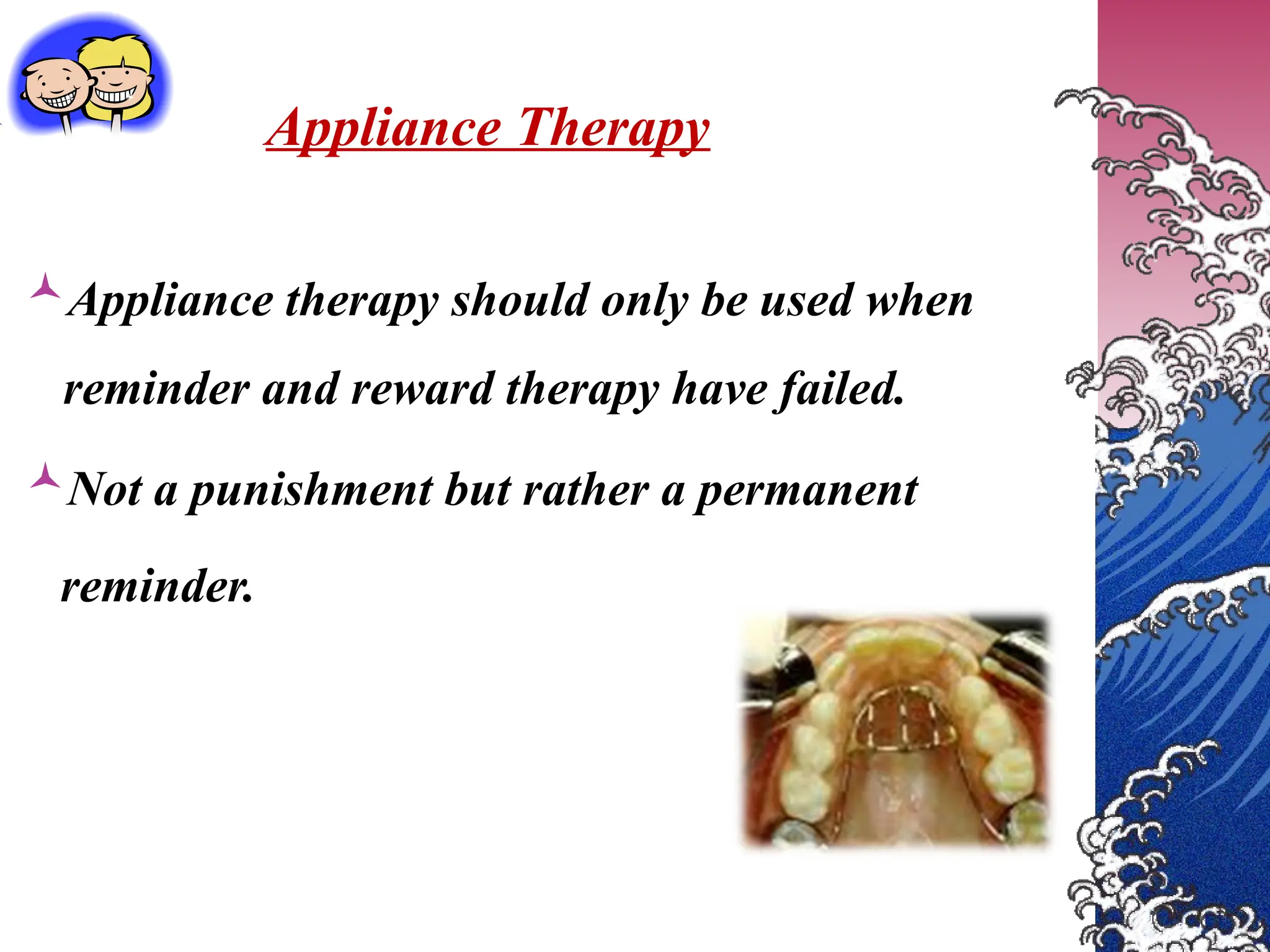
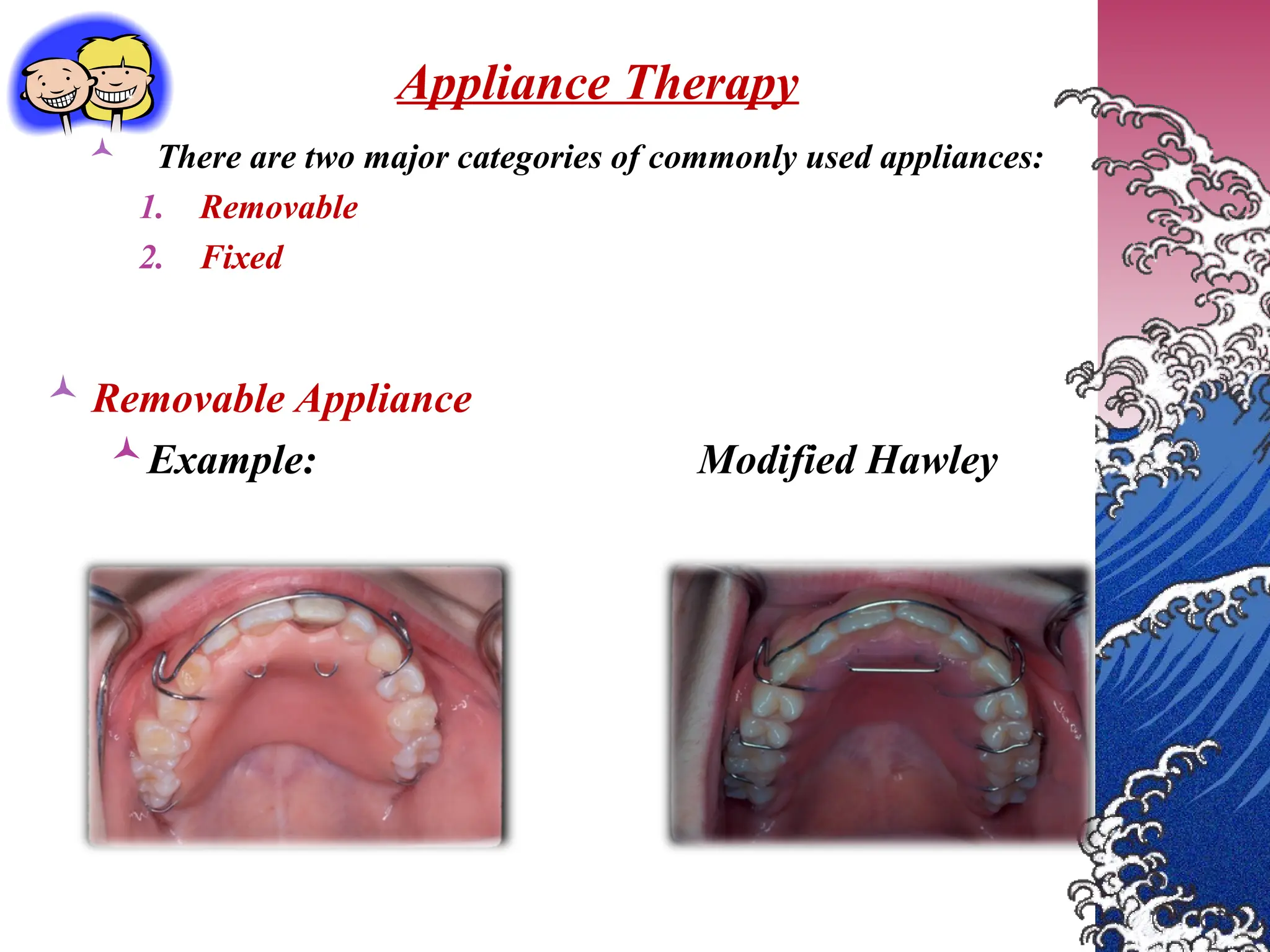
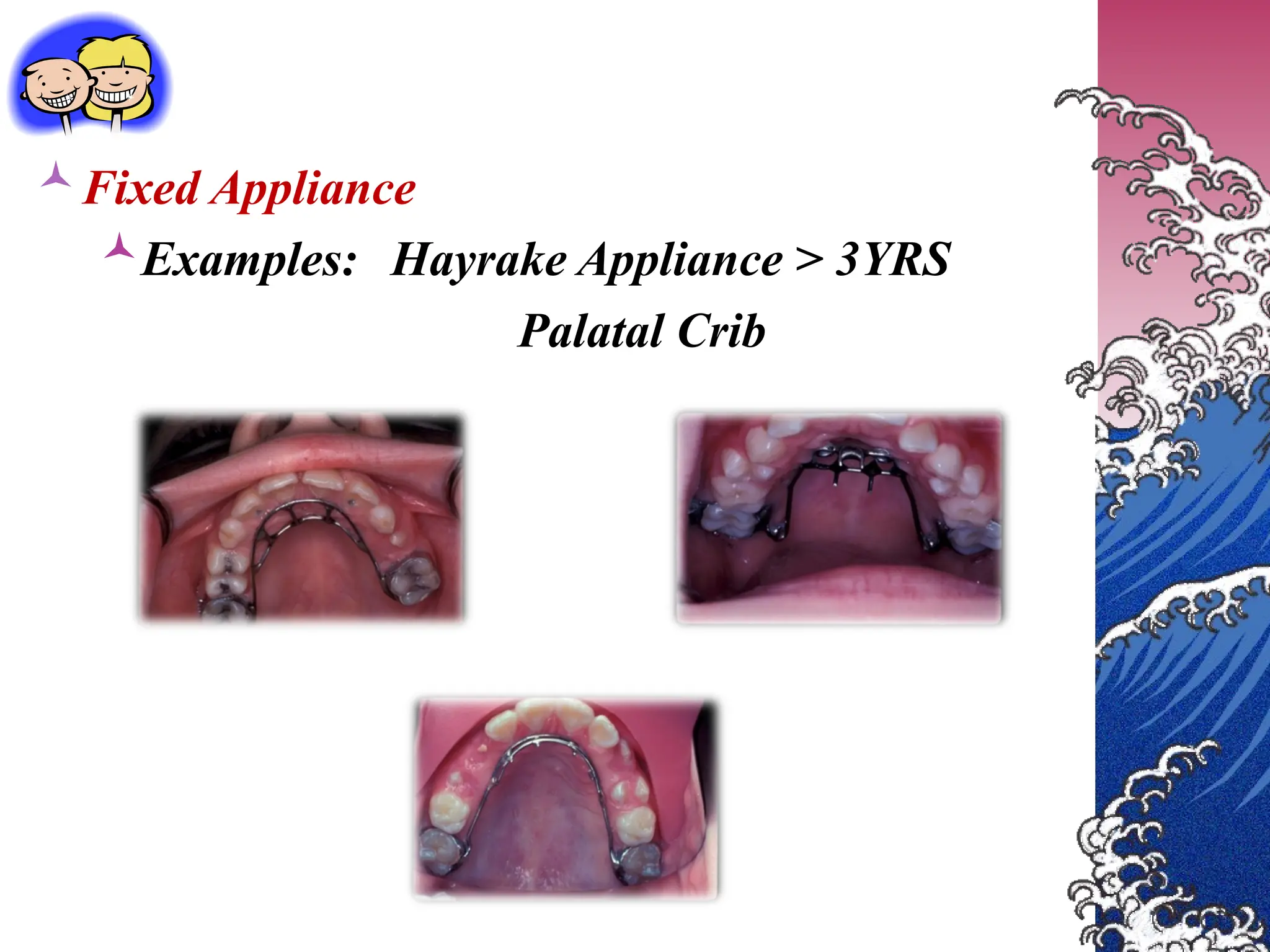
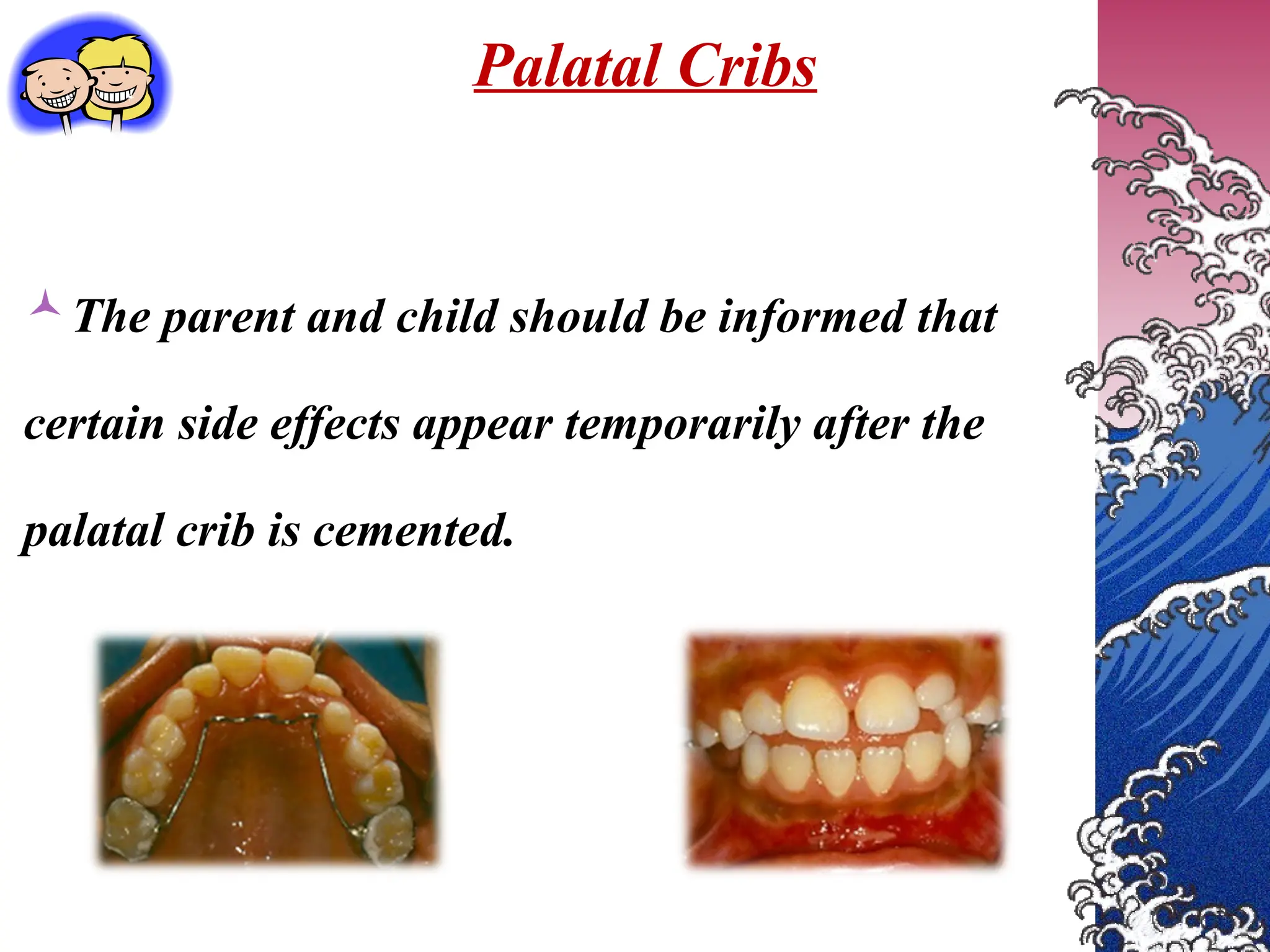
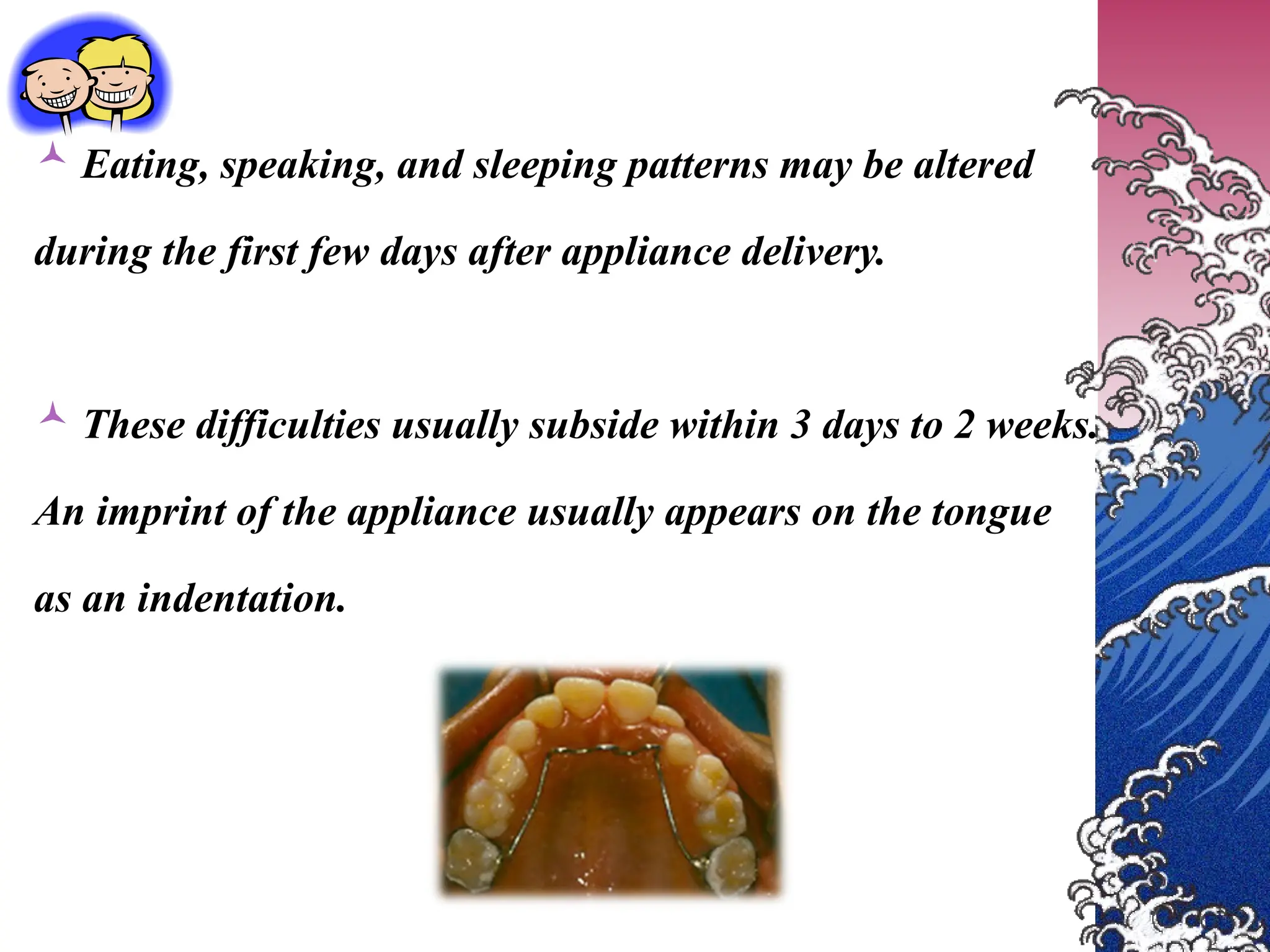
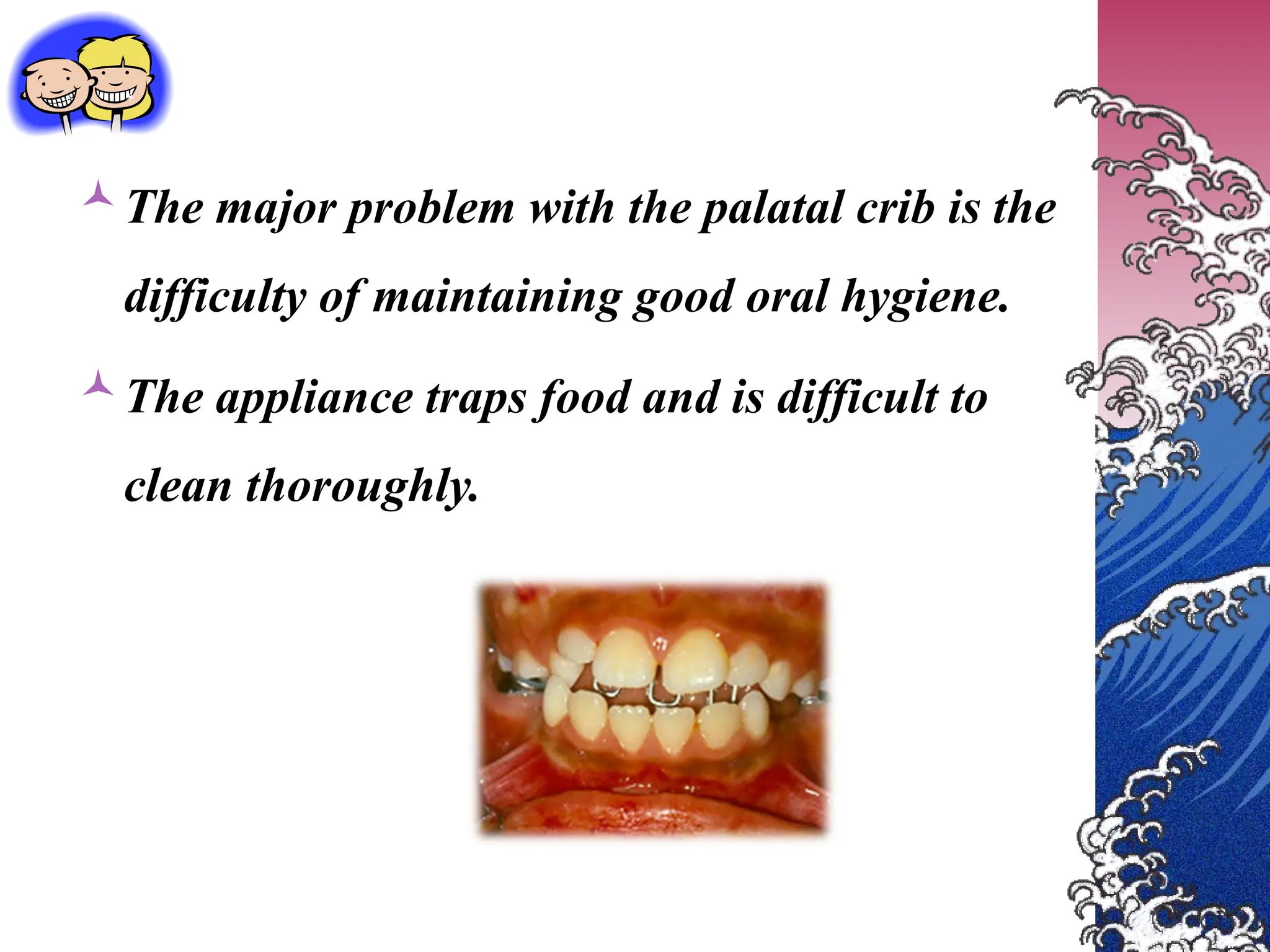
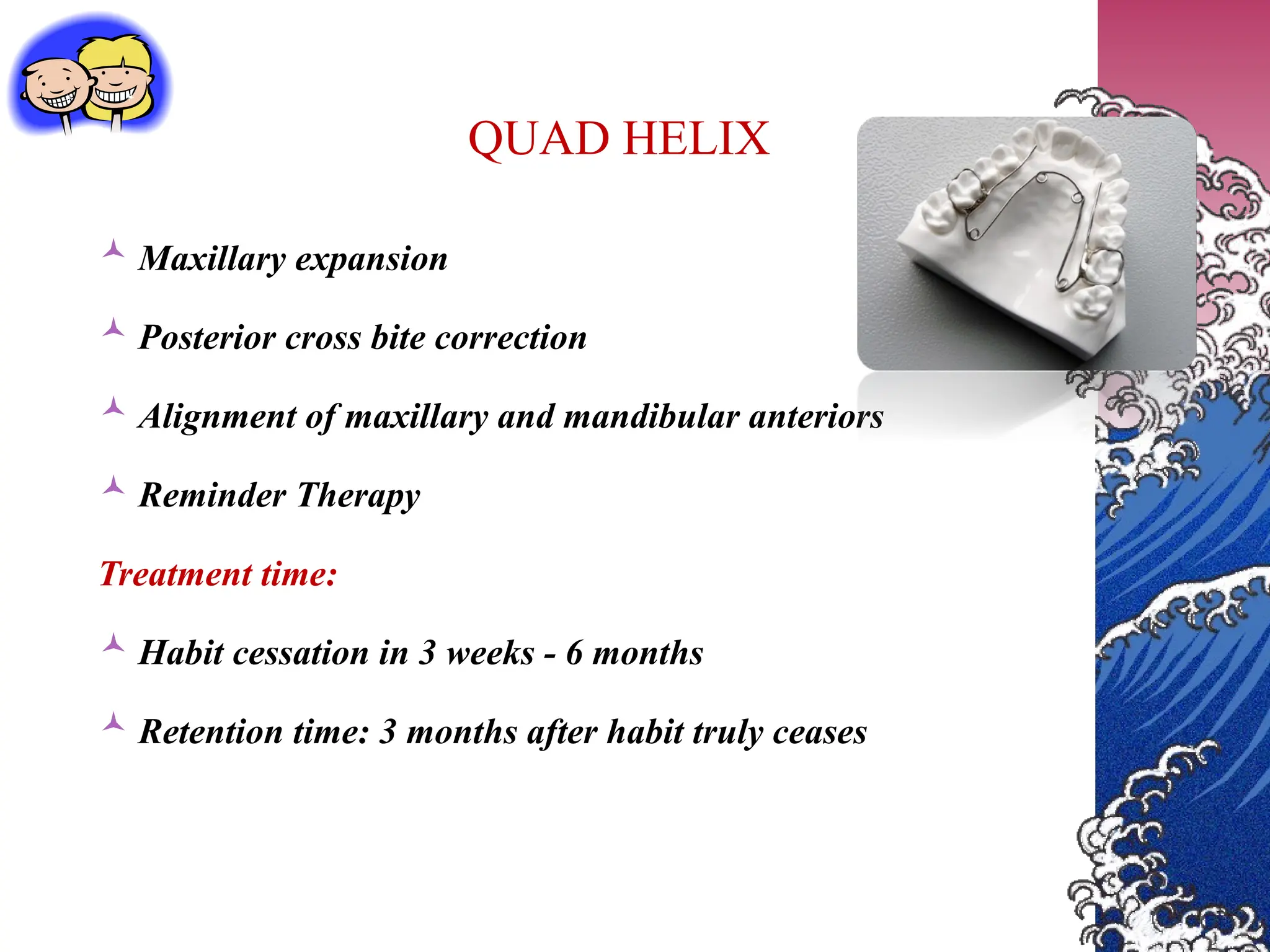
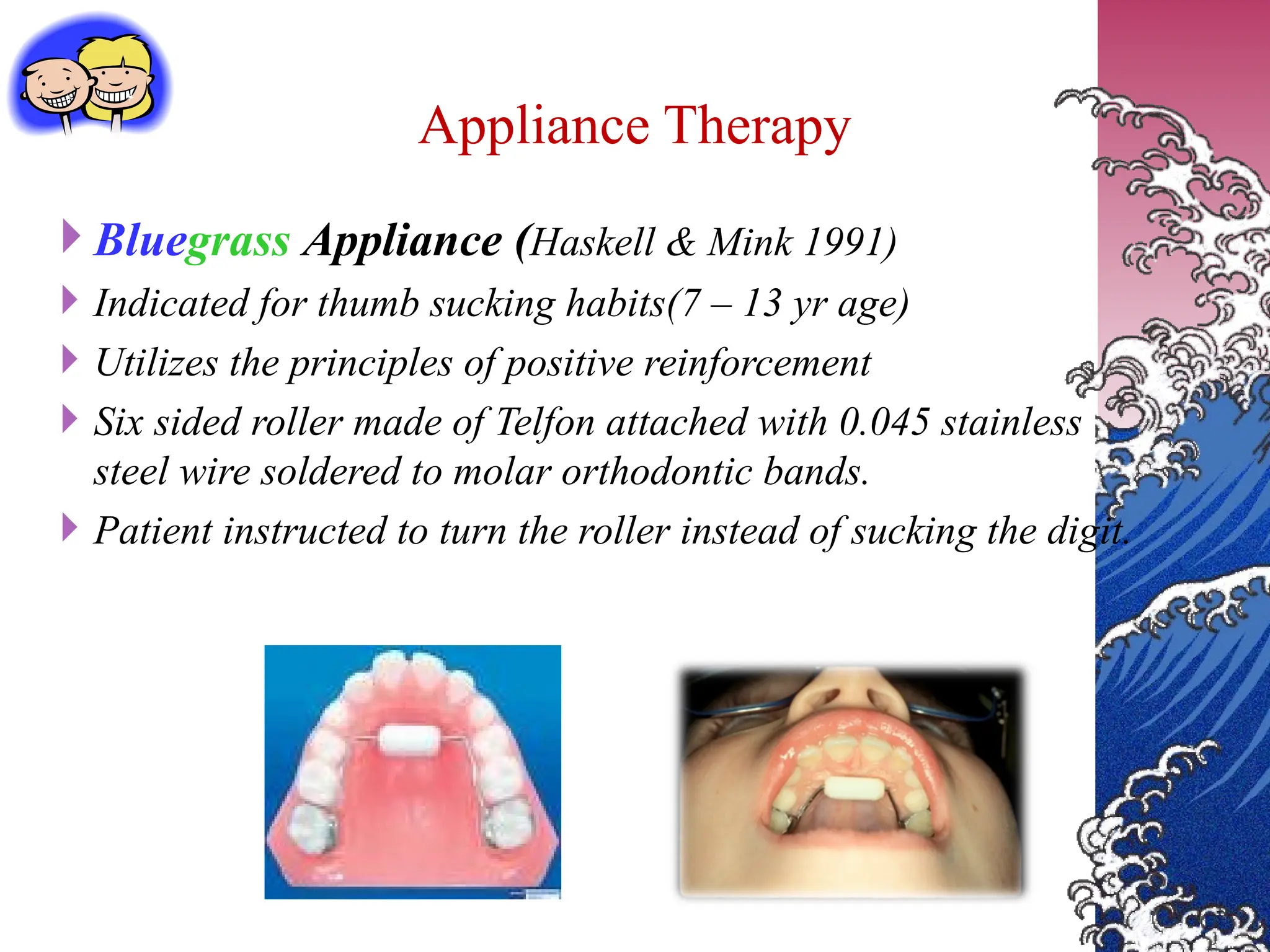
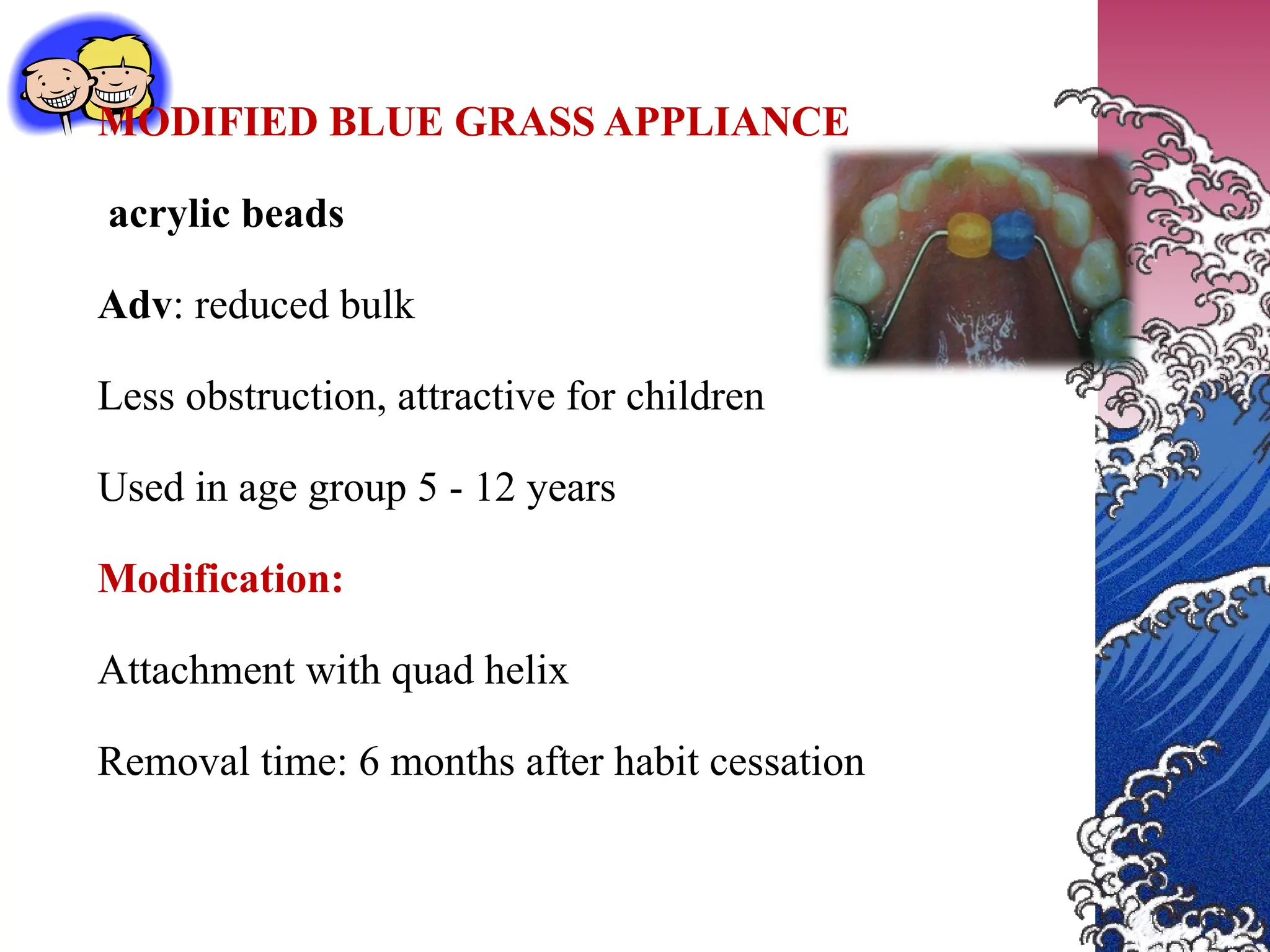
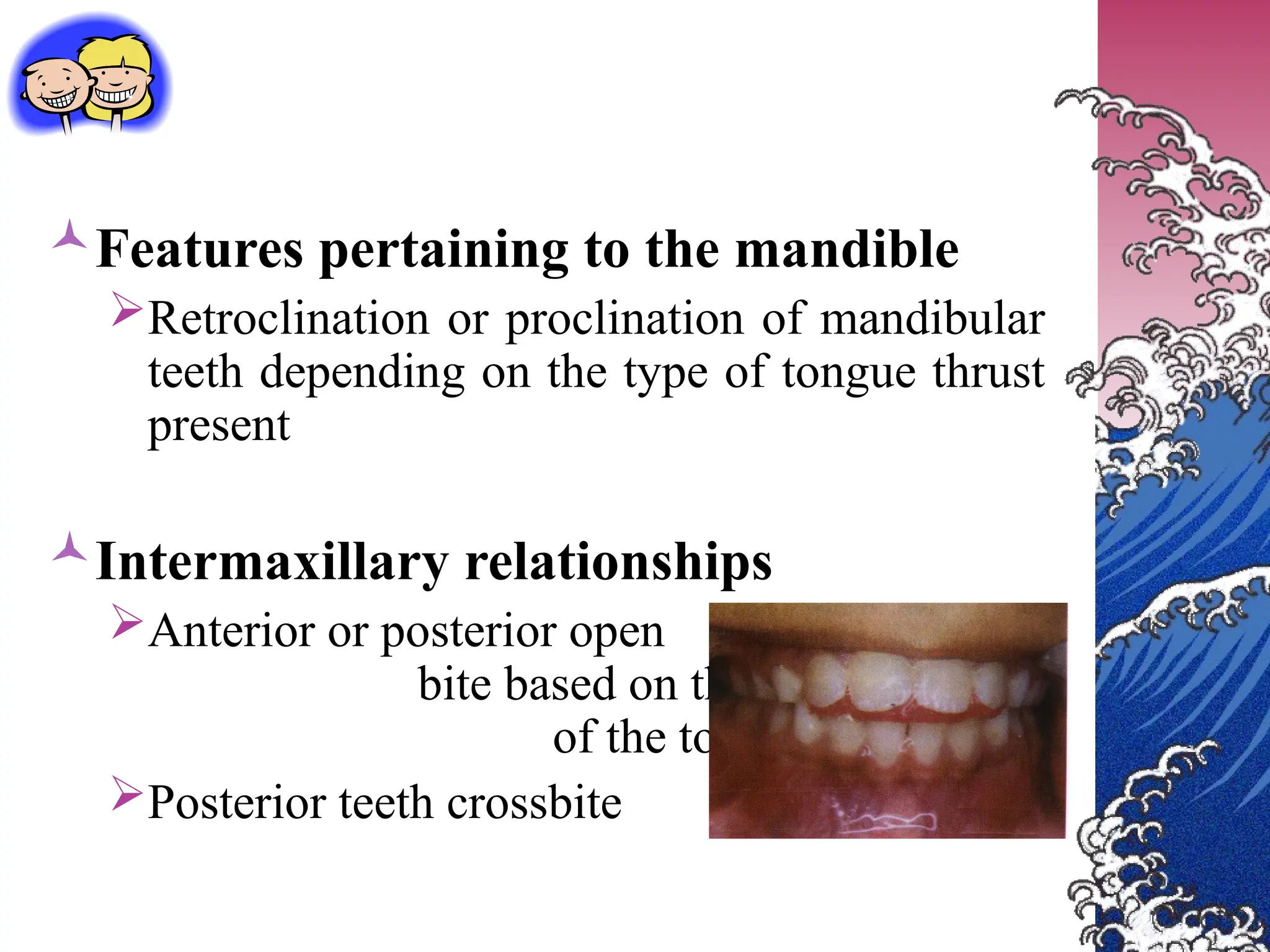
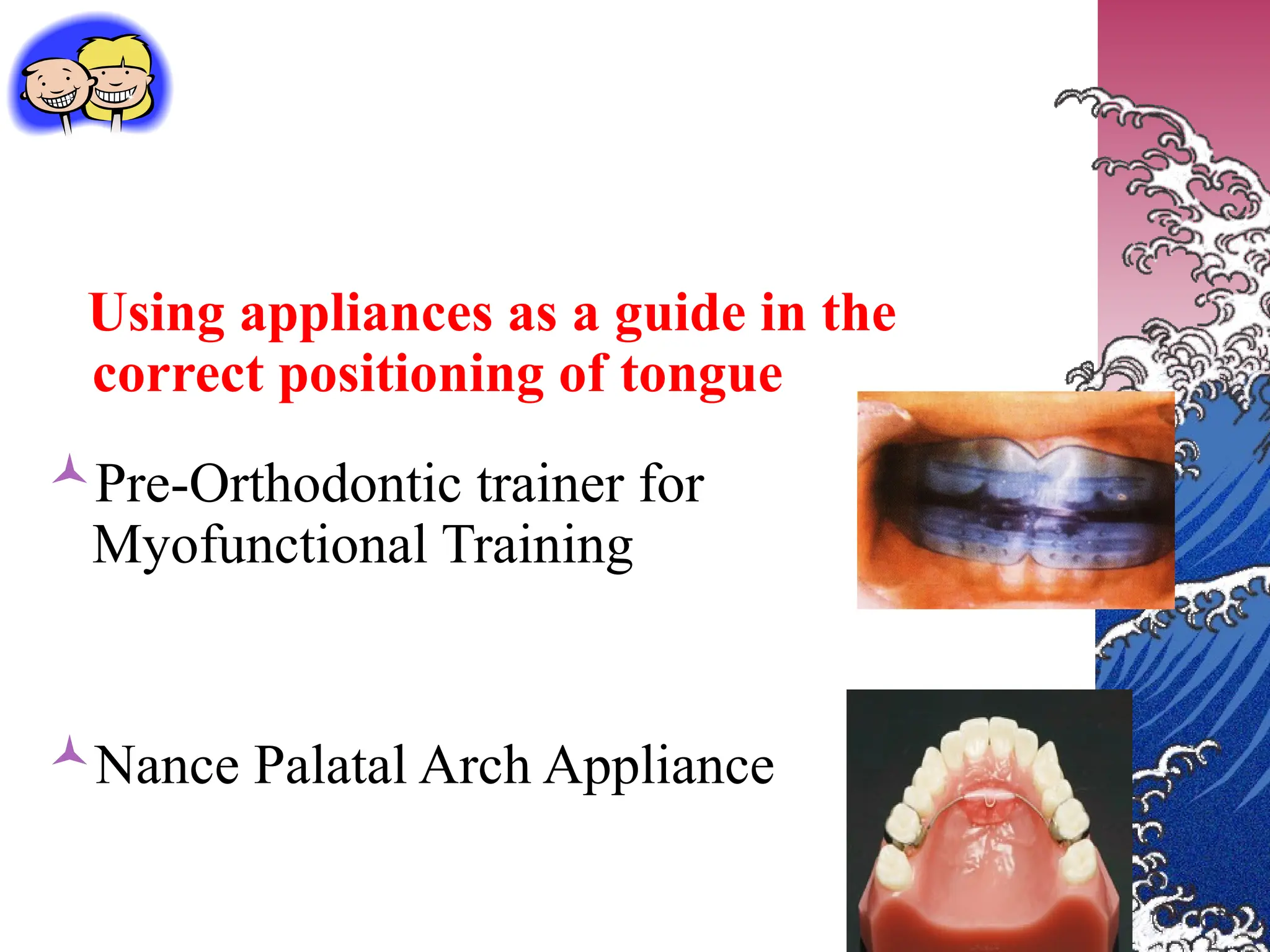
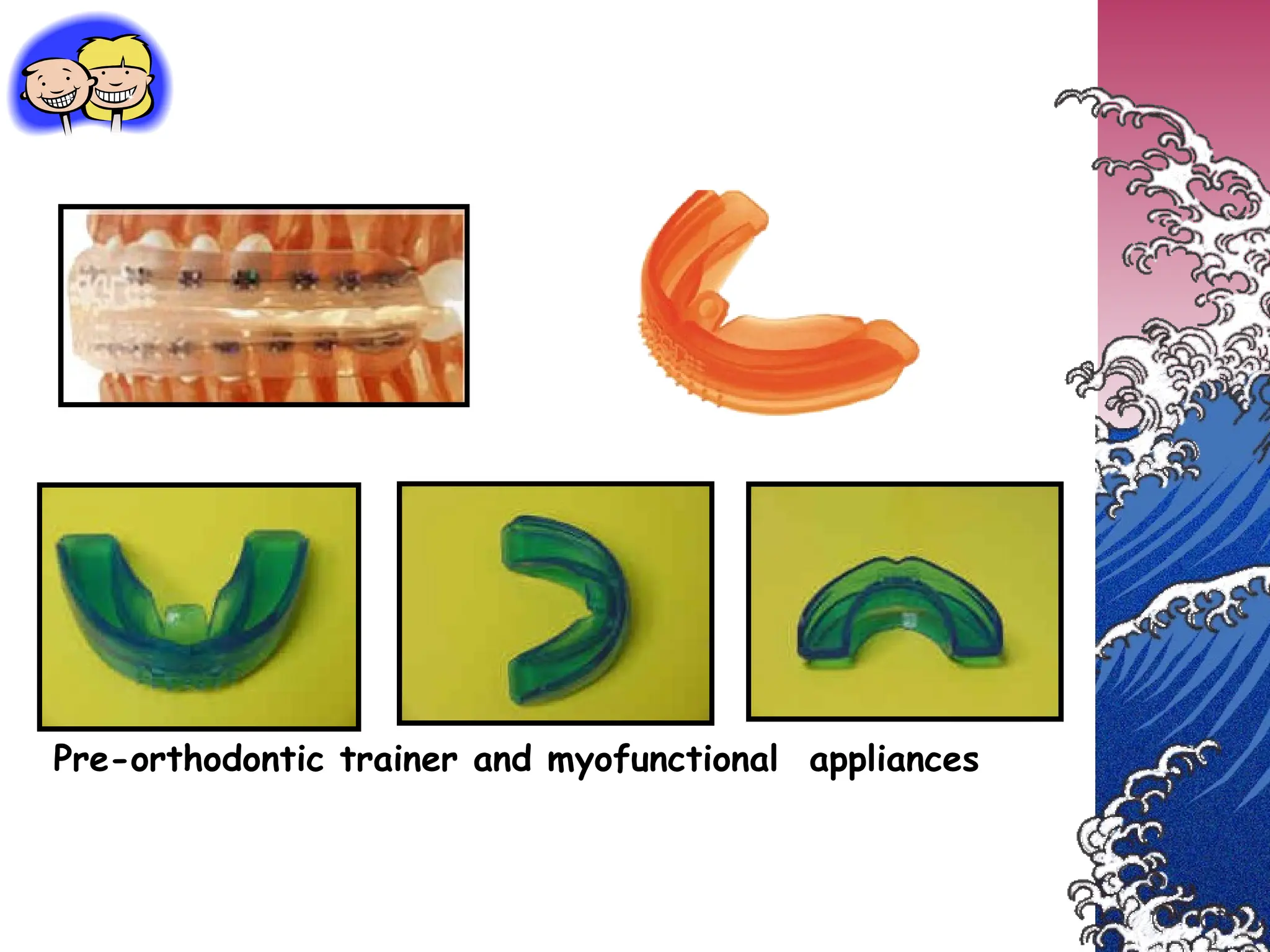
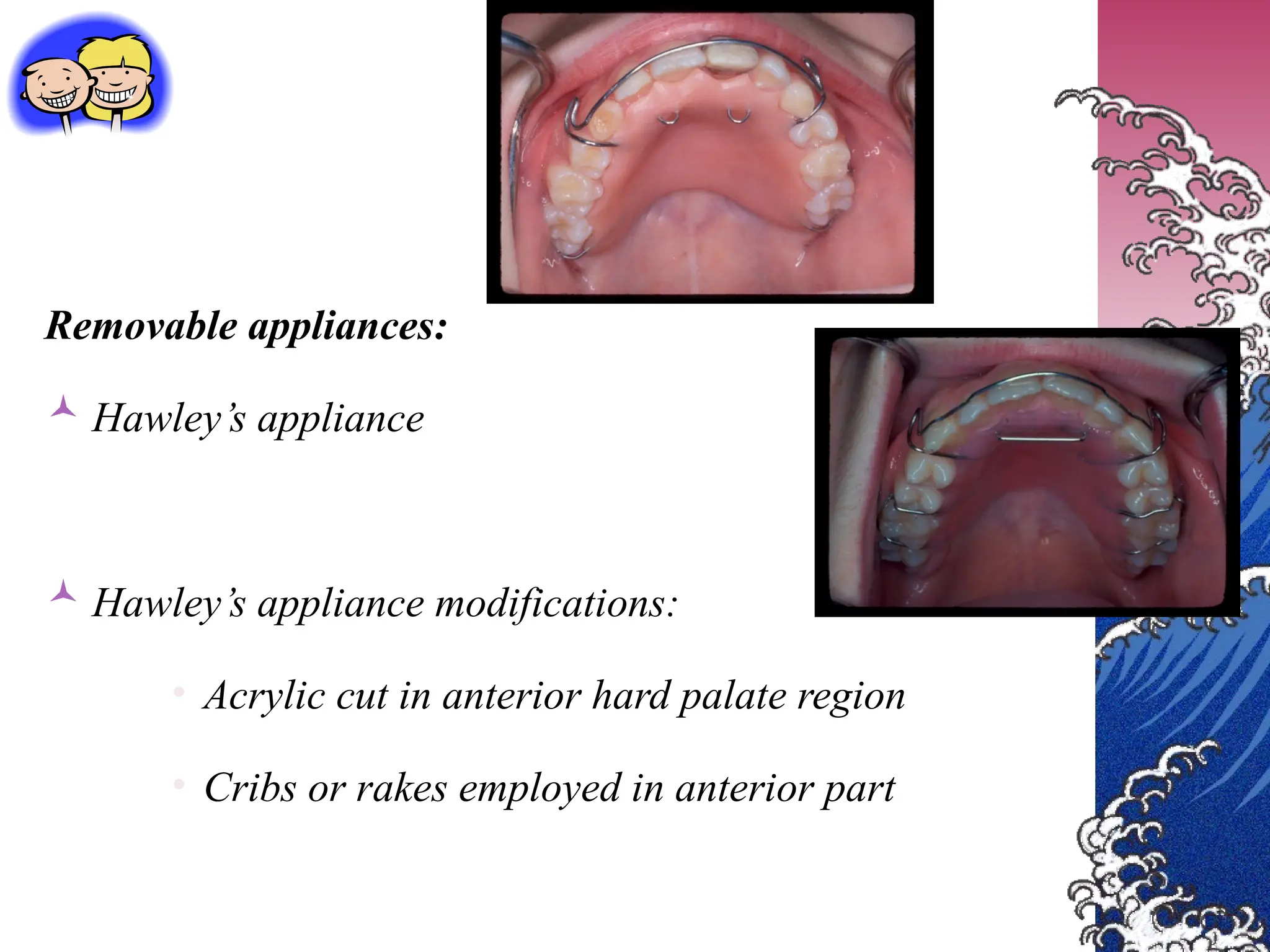
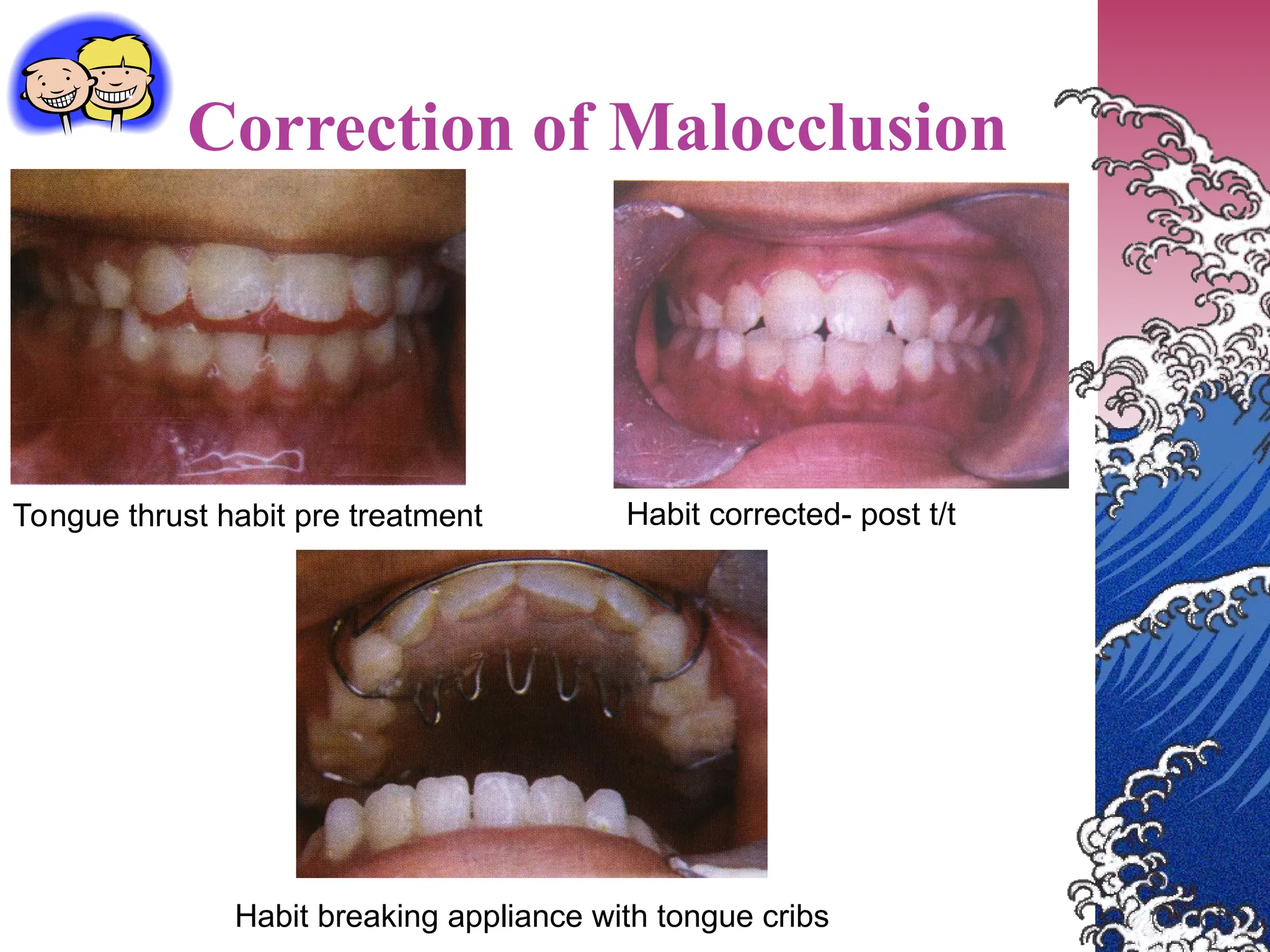
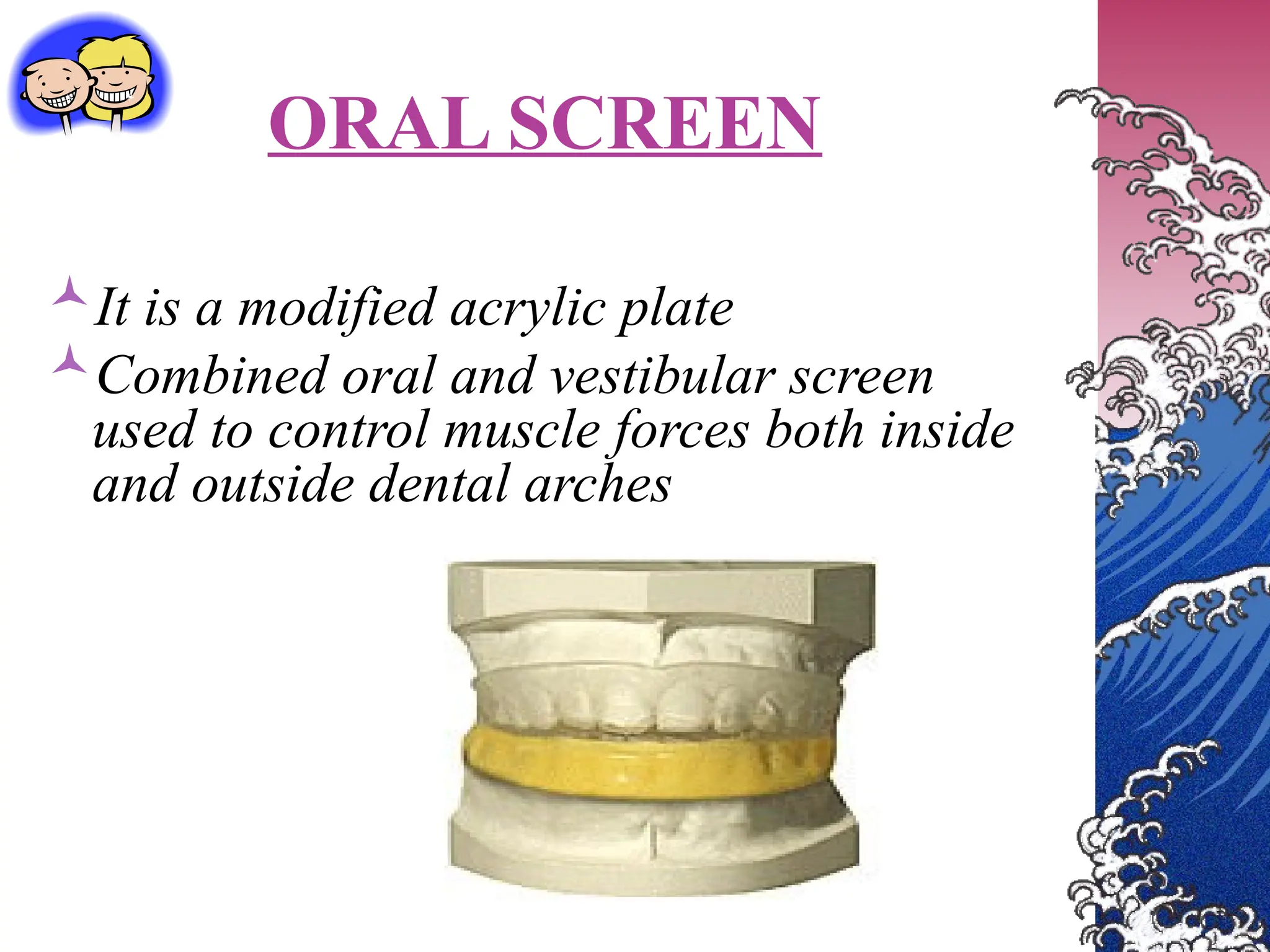
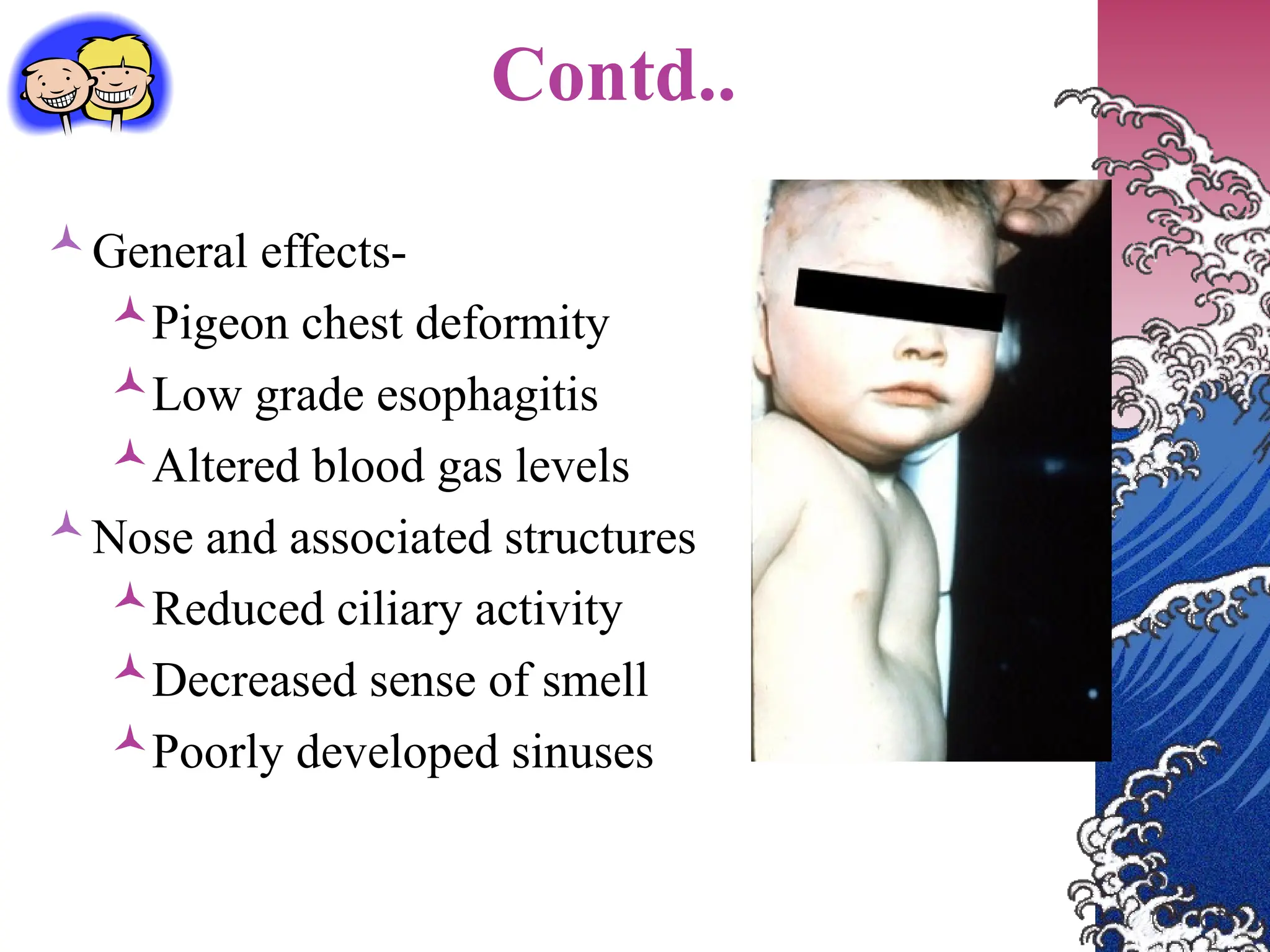
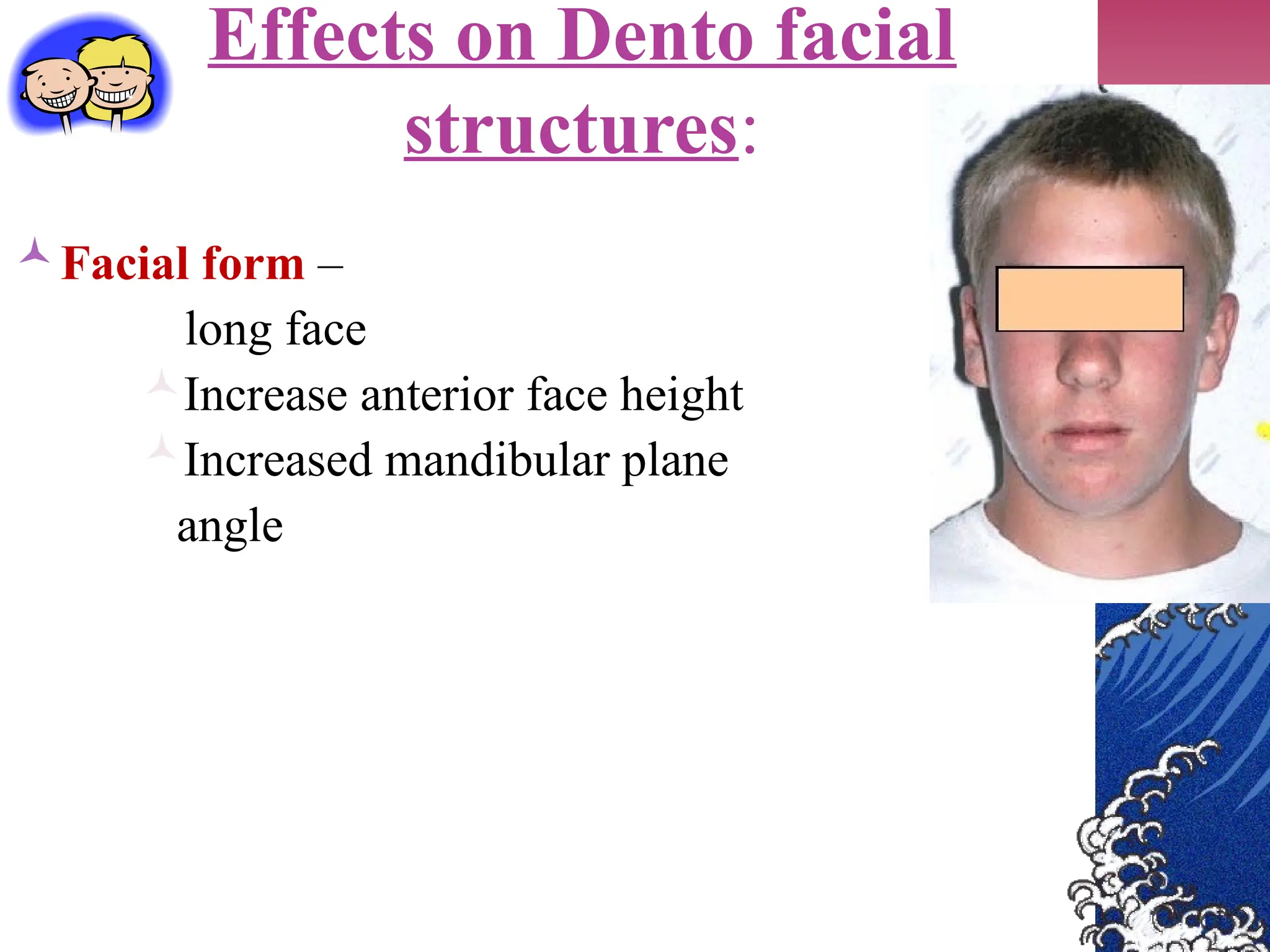
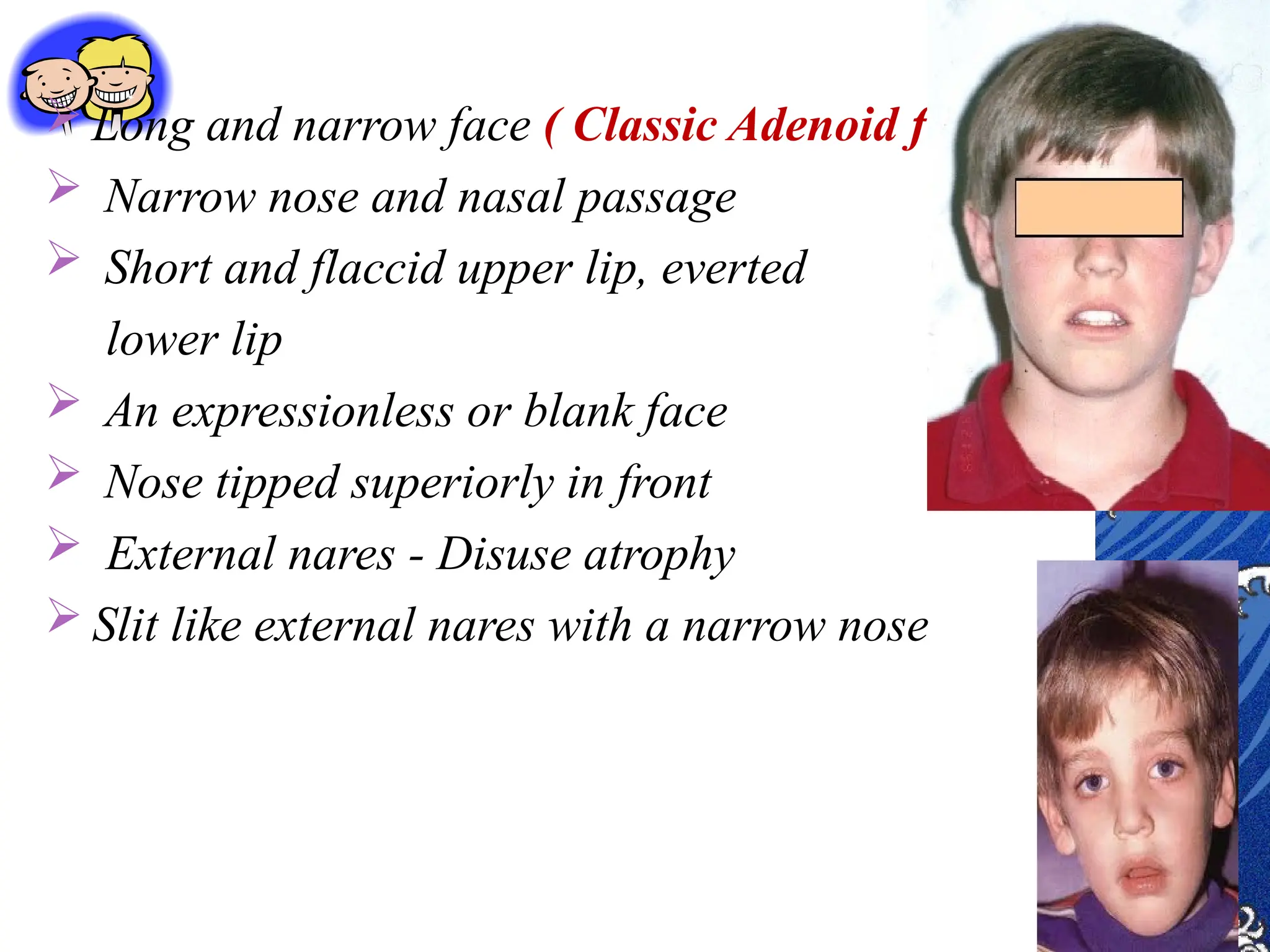
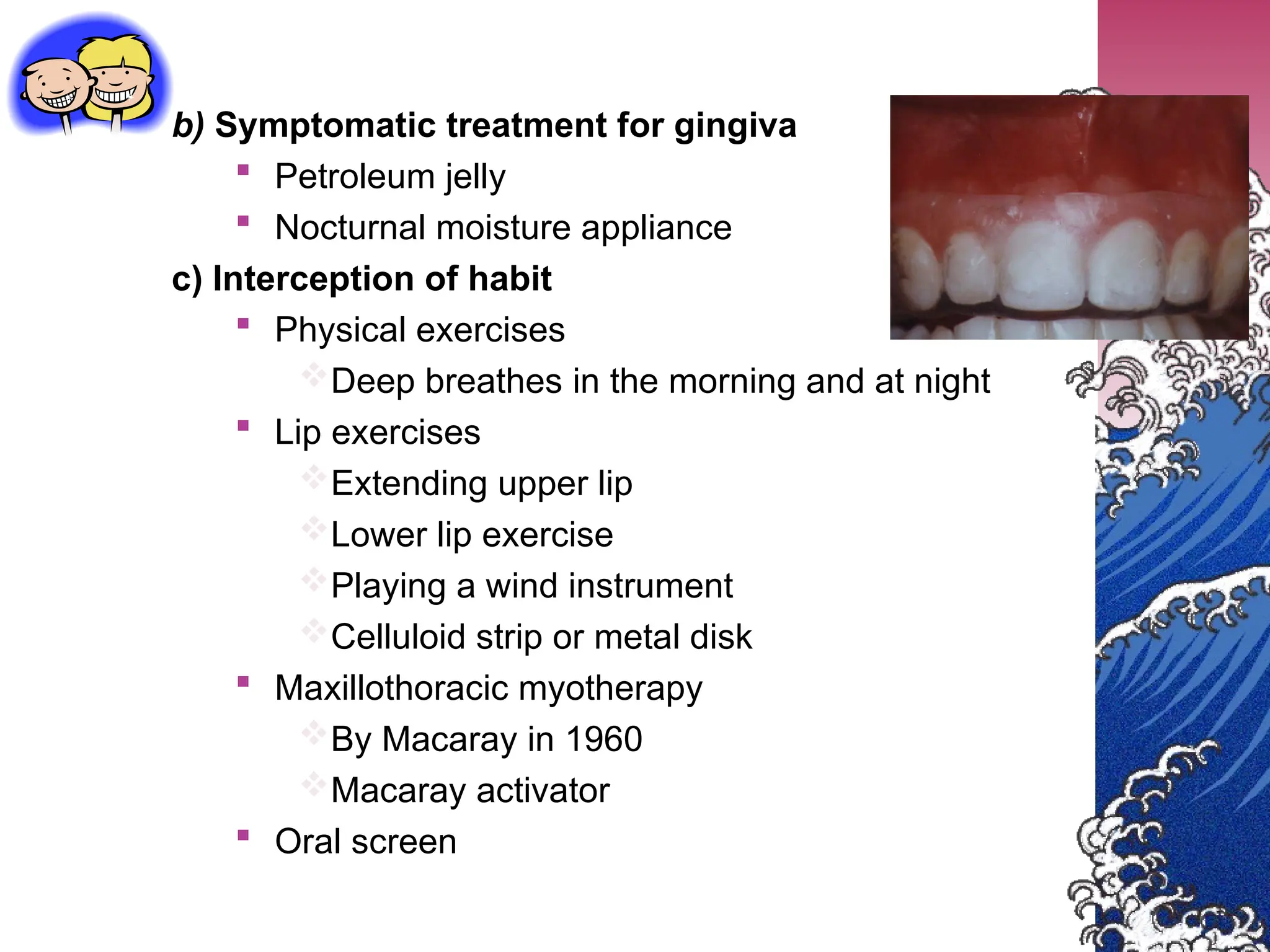
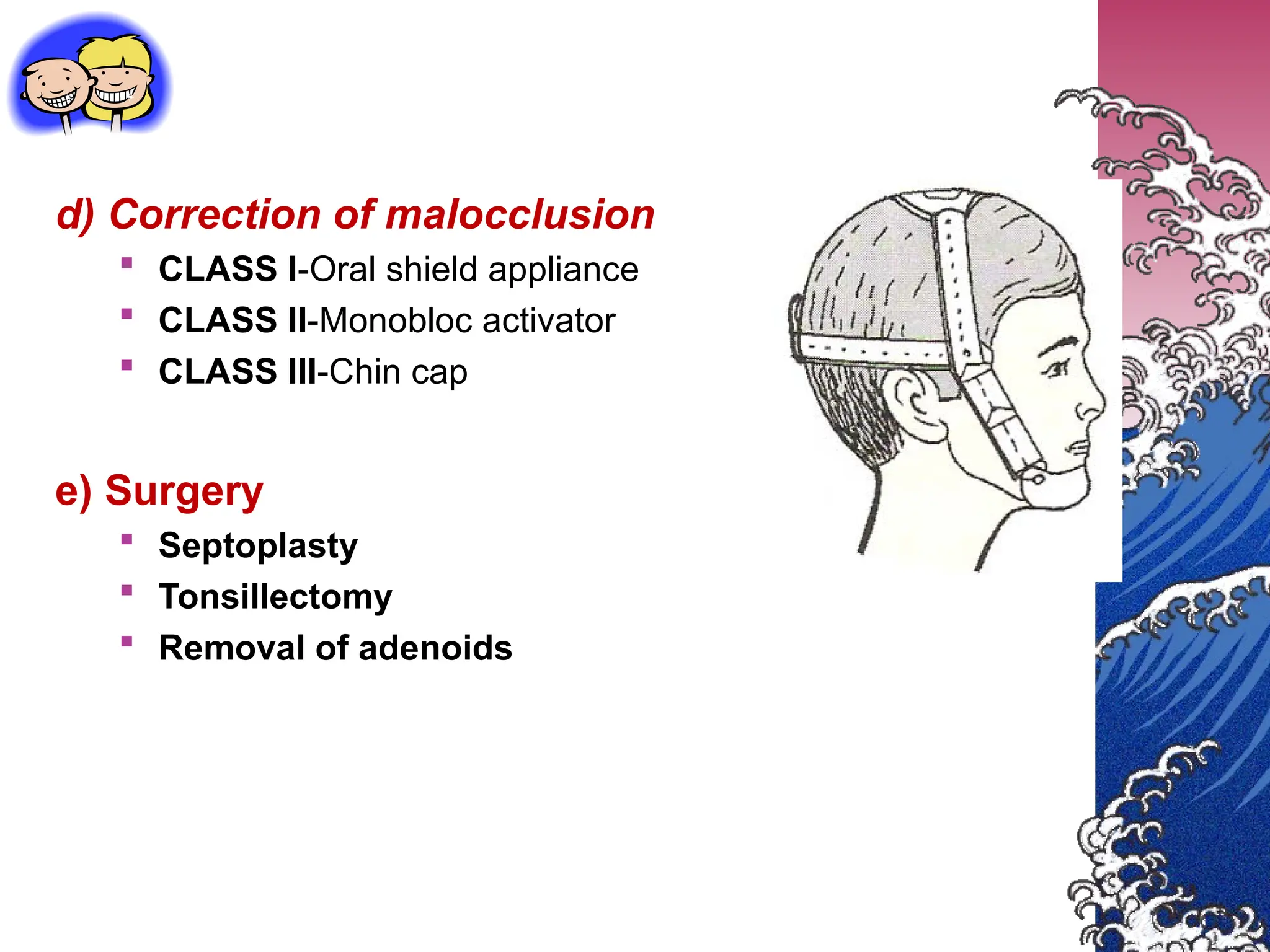
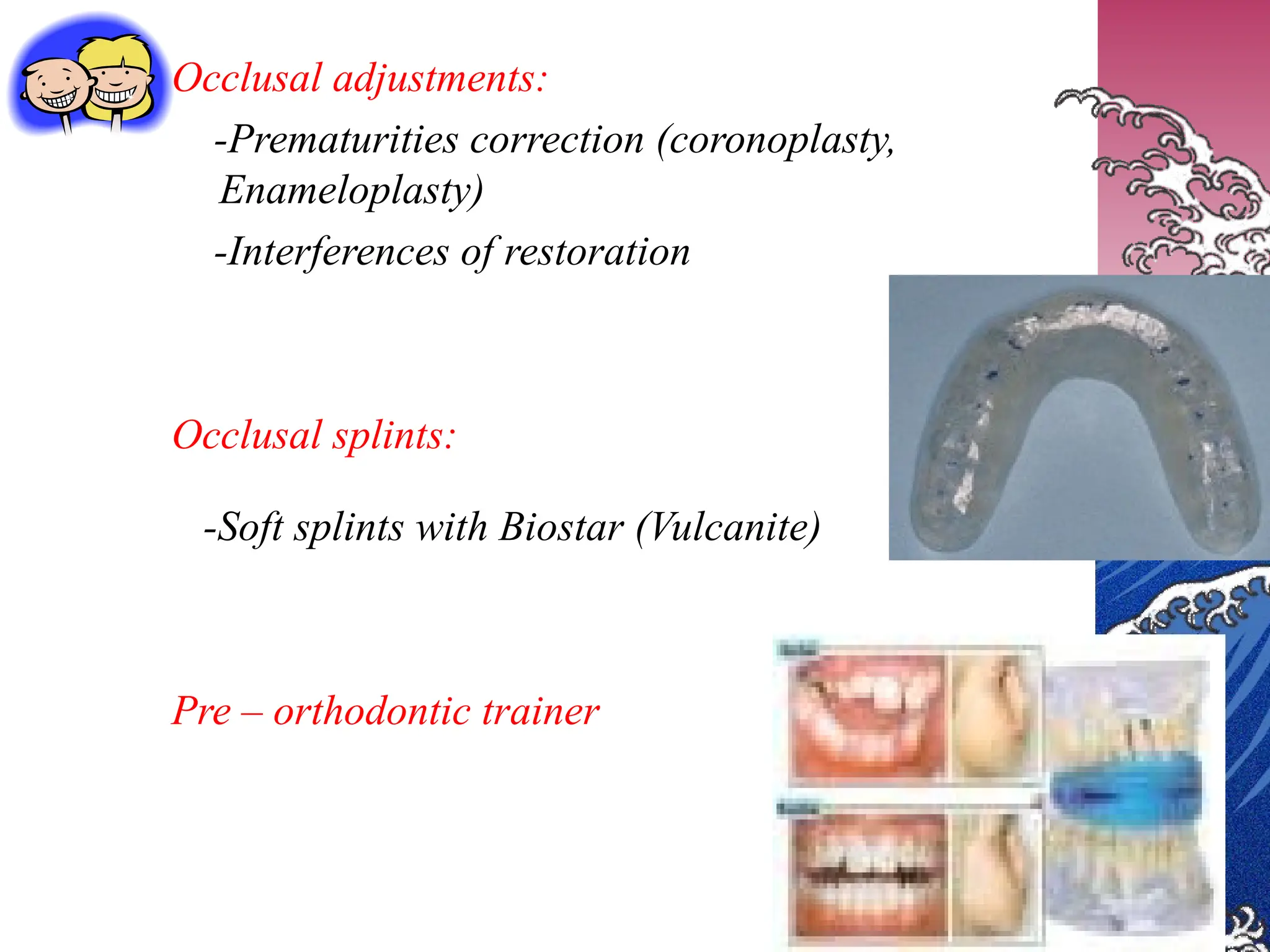
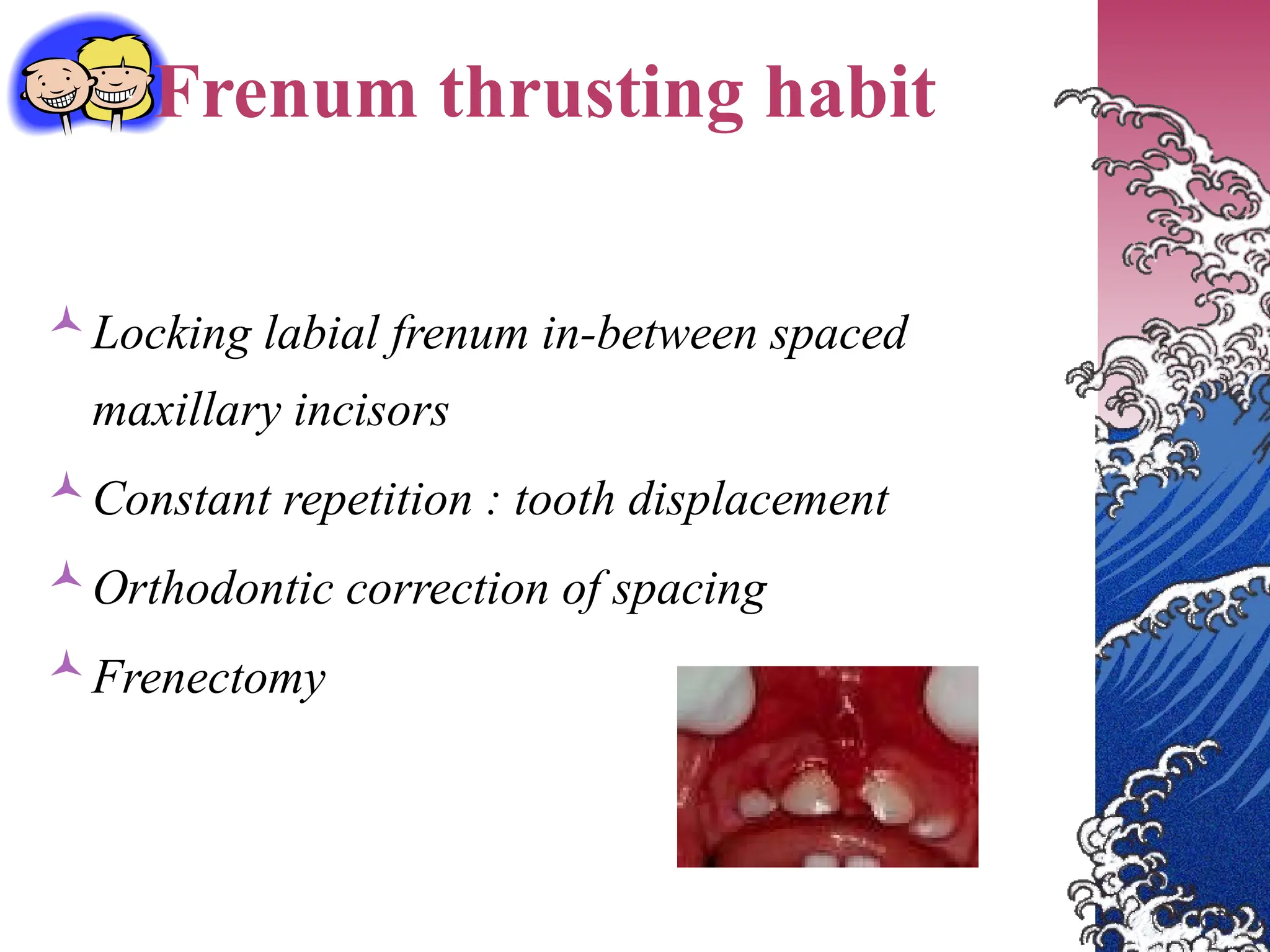
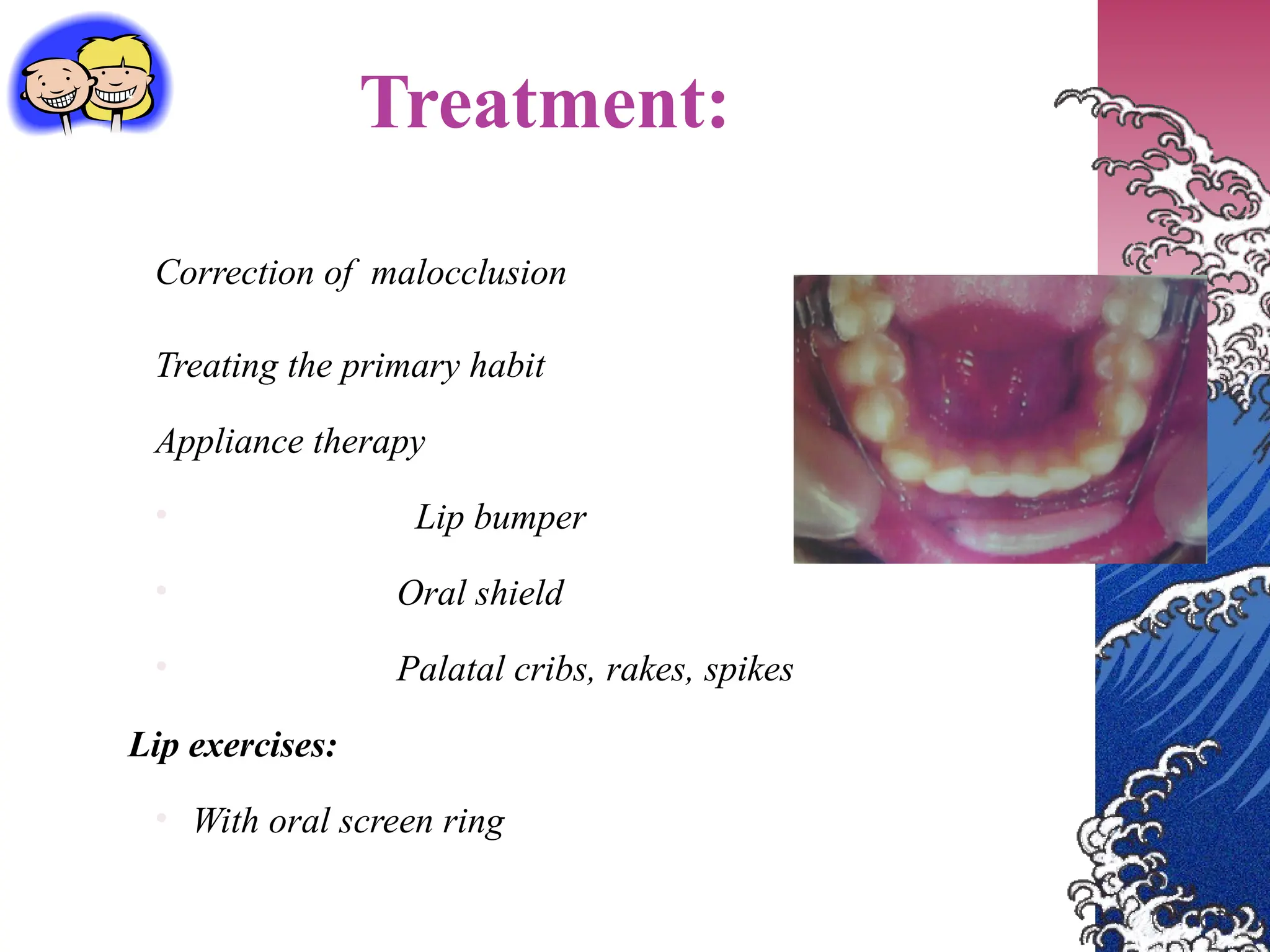
The document discusses various oral habits in children, defining them as repetitive actions impacting dental occlusion and tooth positioning, with distinctions between useful and harmful habits. It classifies these habits into categories such as compulsive and non-compulsive, and outlines impacts on dental health, diagnosis methods, and treatment approaches including psychological therapy and appliance use. Specific habits like thumb sucking and tongue thrusting are examined in detail, highlighting their classifications, etiology, and resultant malocclusions.