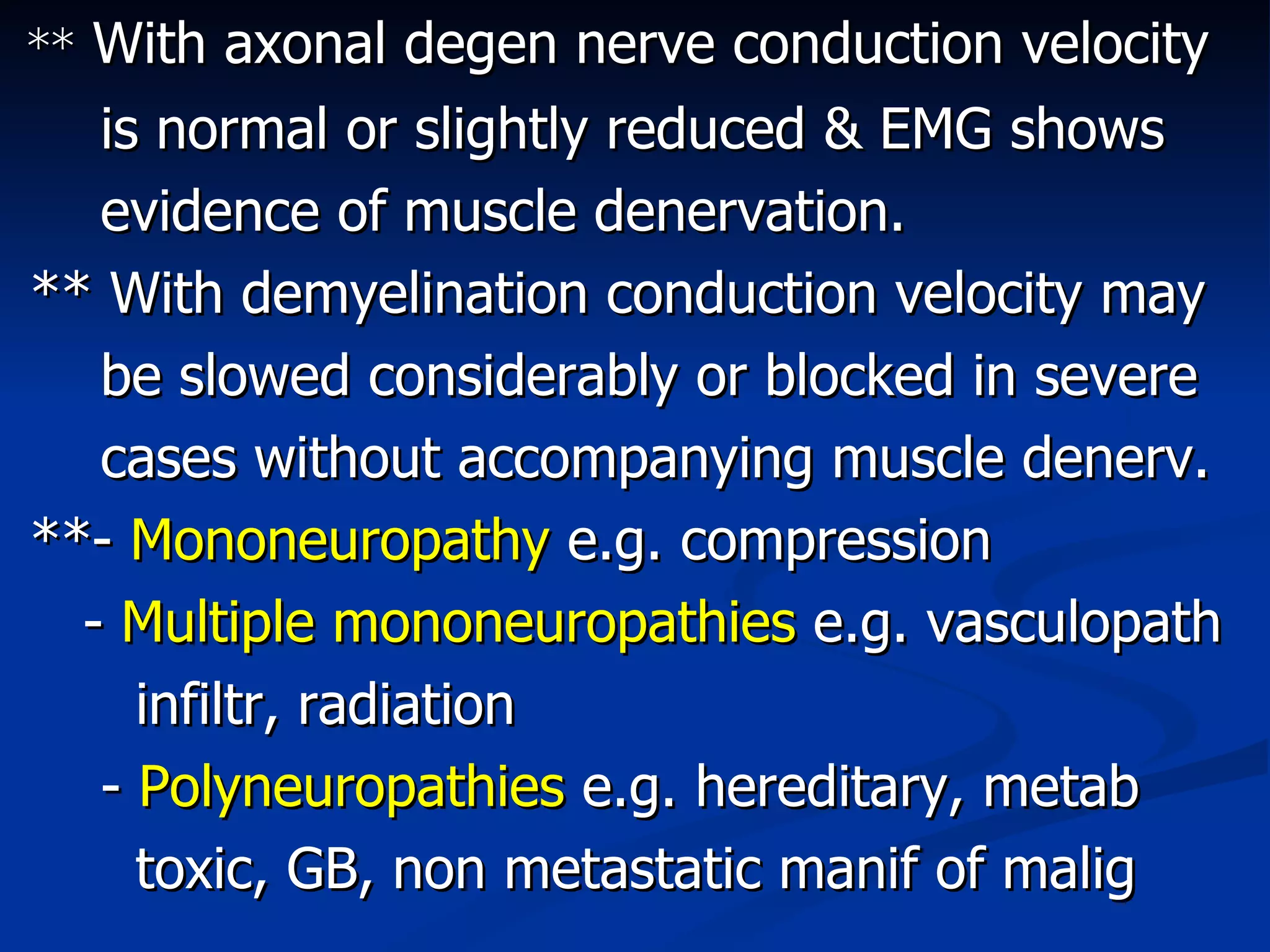
This document discusses peripheral neuropathies and their causes and characteristics. It covers different types of neuropathies including mononeuropathies, mononeuritis multiplex, and polyneuropathies. Common causes of polyneuropathies discussed include inherited conditions, metabolic/endocrine disorders, toxins, infections, inflammation, and vitamin deficiencies. Signs and symptoms and investigative approaches are also summarized.