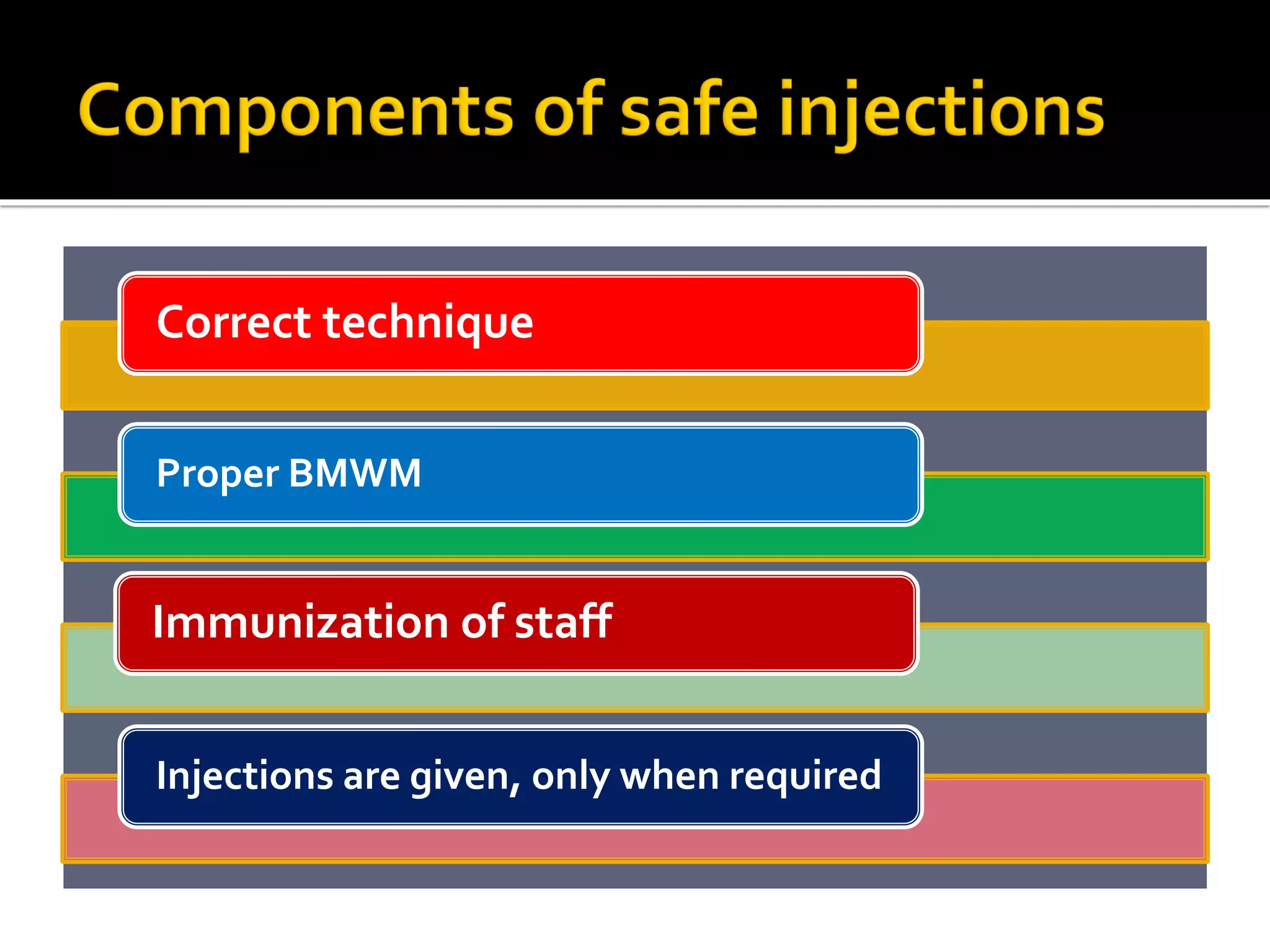
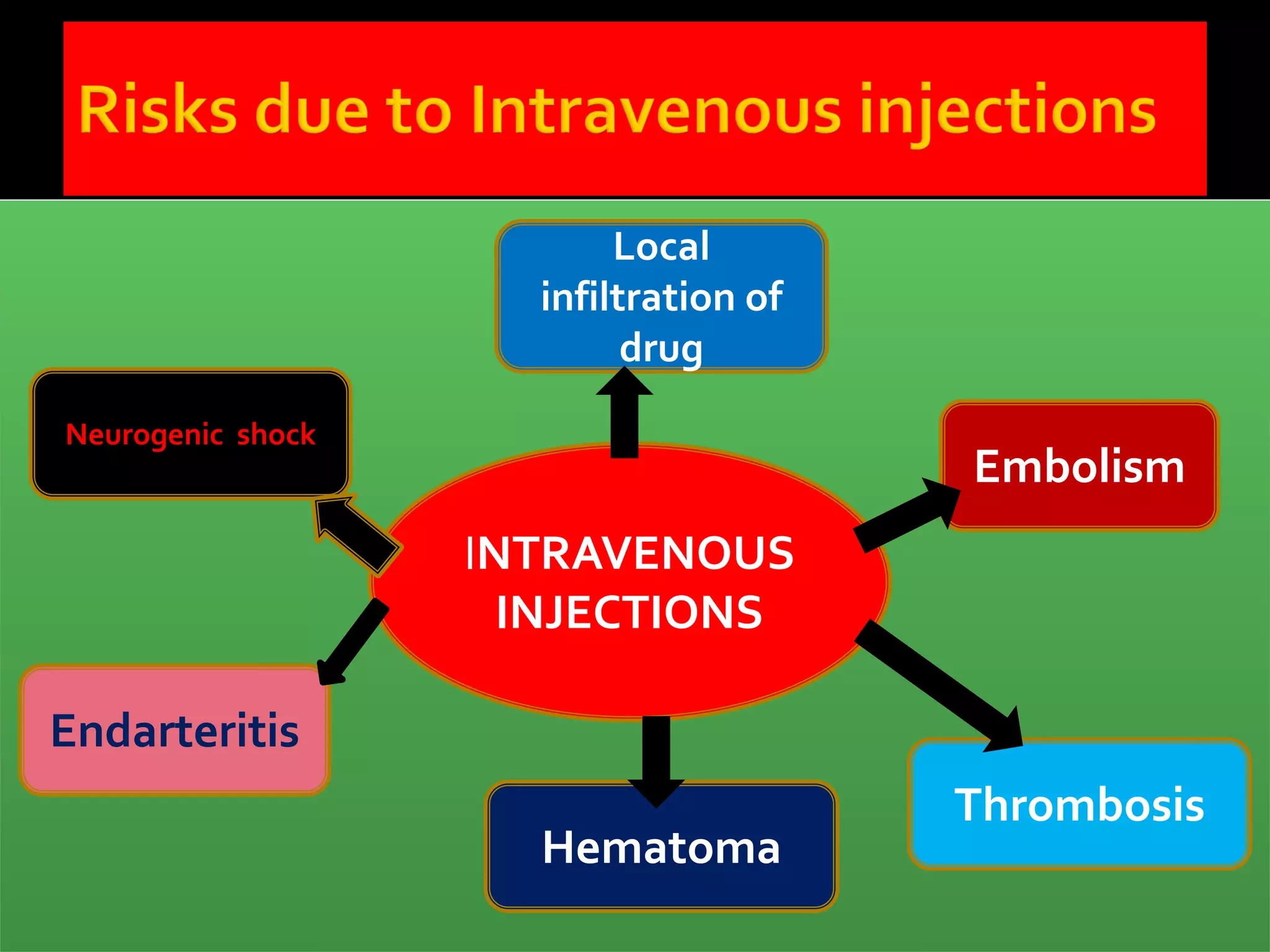
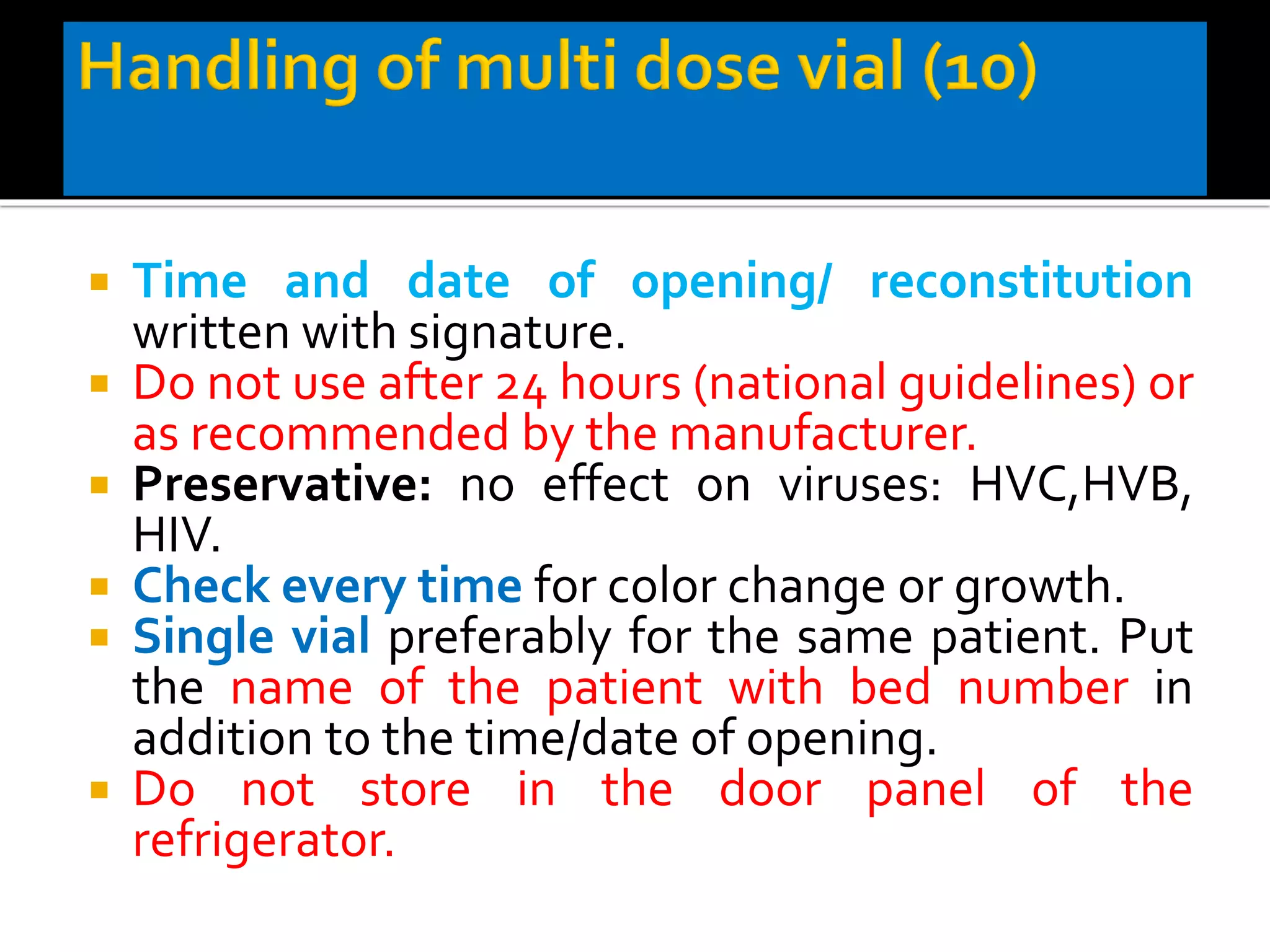
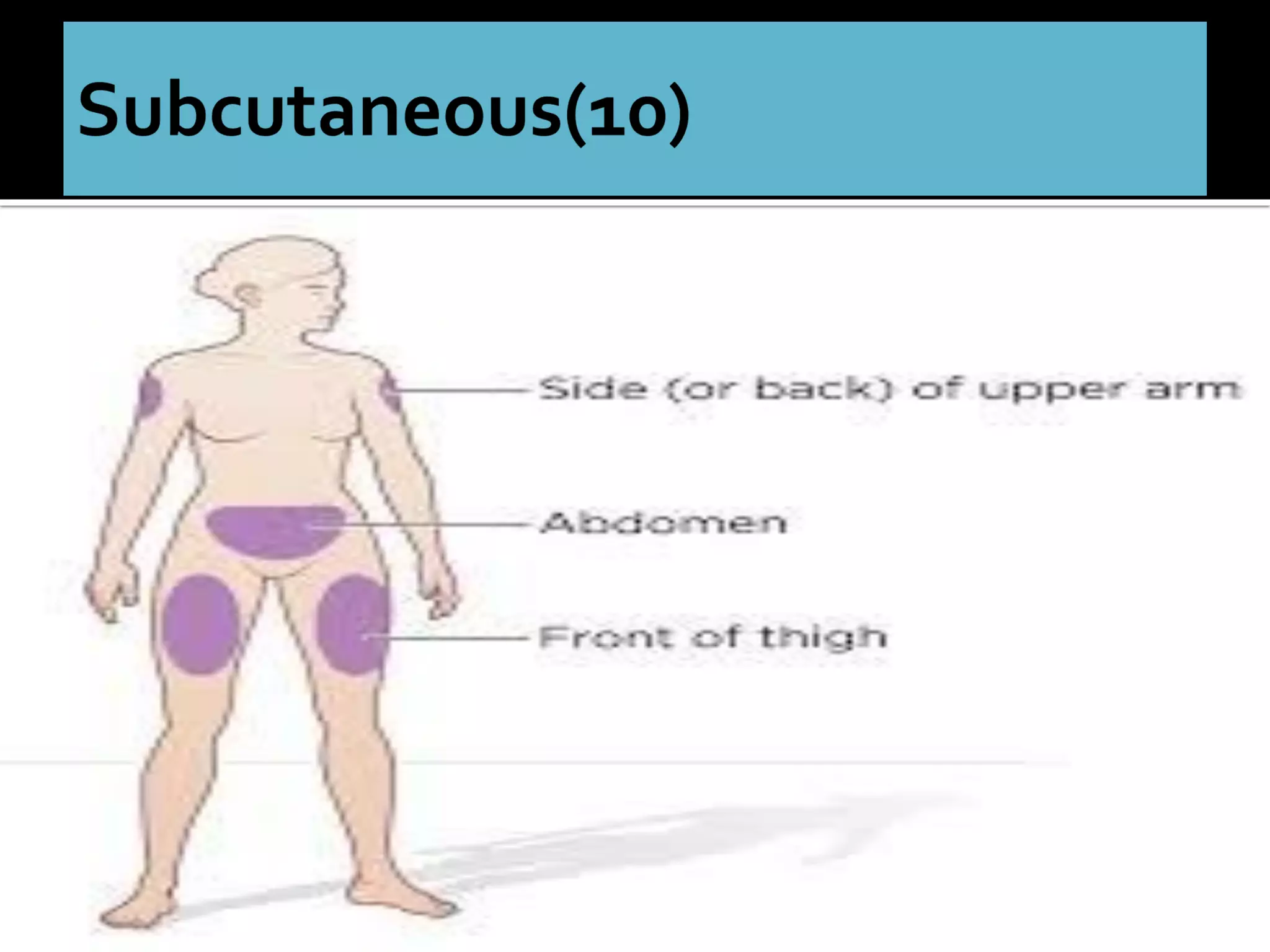
The document discusses the prevalence of unsafe injection practices in India, highlighting significant statistics related to infections like hepatitis and HIV due to inadequate sterilization and reuse of syringes. It emphasizes the importance of safe injection practices, proper biomedical waste management, and the role of healthcare professionals in educating patients about the necessity and techniques of injections. Guidelines have been issued to improve safety, reduce unnecessary injections, and ensure community awareness to mitigate health risks associated with injection use.