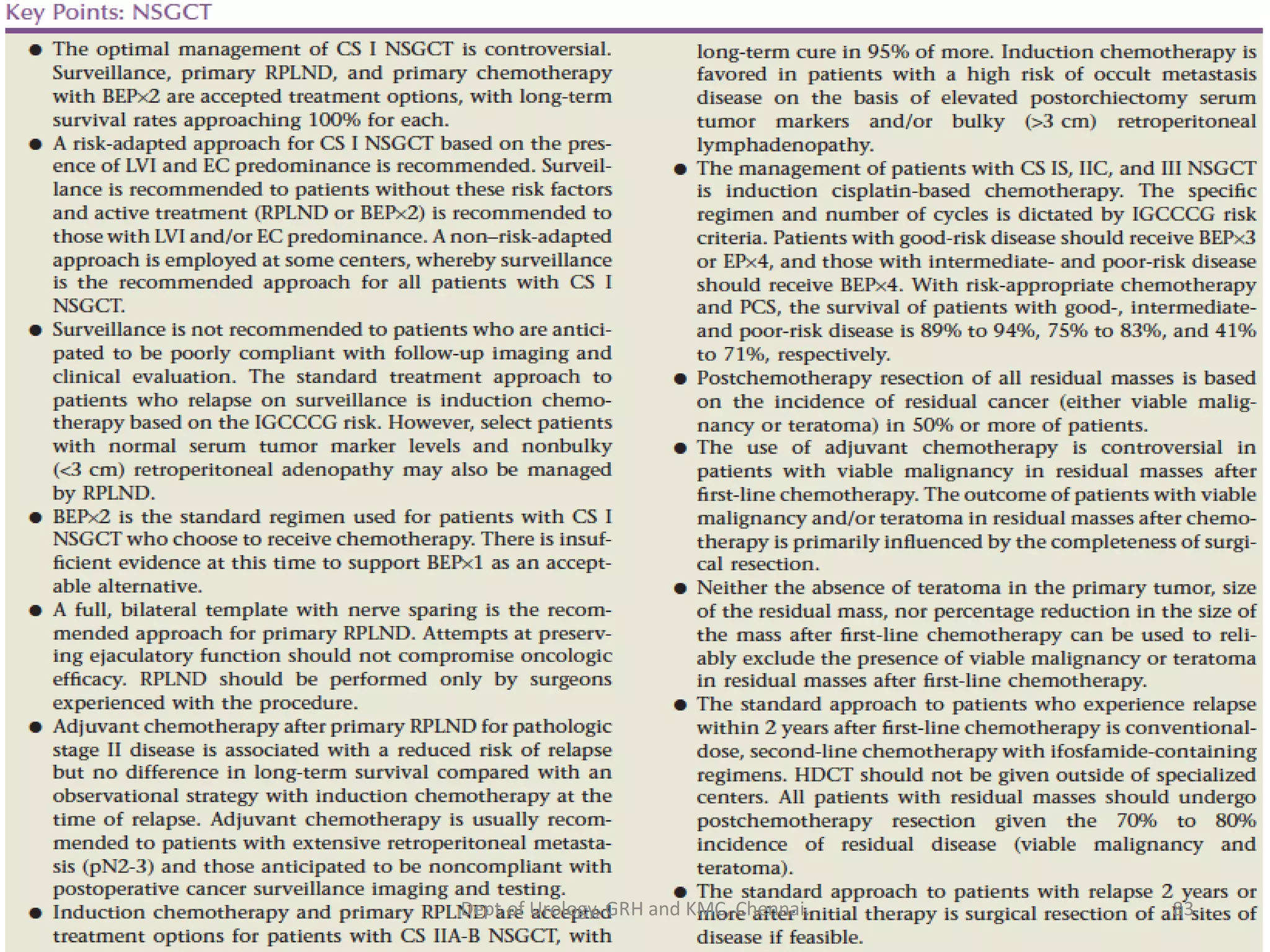
This document discusses the management of non-seminomatous germ cell tumors (NSGCTs). It covers the pathological classification, clinical staging, treatment approaches for different stages, and management of residual or relapsed disease. For stage I disease, options include observation, retroperitoneal lymph node dissection (RPLND), or chemotherapy depending on risk factors. For stage II, nerve-sparing RPLND or chemotherapy is recommended based on tumor burden. Stage III usually receives chemotherapy followed by RPLND if needed. Common regimens include BEP and salvage therapies like TIP are discussed for relapsed or refractory cases. The roles of surgery, chemotherapy, surveillance and newer agents are outlined.




































![[18F]-FDG-PET in Germ Cell Tumors following Chemotherapy:
Results of the German Multicenter Trial
n= 141
NPV
Negative
predictive value
PPV
Positive
predictive value
ACC
Accuracy
CT
95% CI
0% 51%
43; 60%
51%
43; 60%
PET
95% CI
59%
44; 72%
57%
46; 67%
57%
49; 66%
M. De Wit, ASCO 2006, abstract # 4521
Statistical plan: estimate of >70% accuracy for PET
37
Dept of Urology, GRH and KMC, Chennai.](https://image.slidesharecdn.com/testis-carcinoma-management-nsgct-210610131153/75/Testis-carcinoma-management-nsgct-37-2048.jpg)